Post-radiation lesions are a favorable prognostic factor in diffuse glioma
Arthur T.J. van der Boog,
The Netherlands
PD-0244
Abstract
Post-radiation lesions are a favorable prognostic factor in diffuse glioma
Authors: Arthur van der Boog1, Szabolcs David1, Fia Cialdella1,2, Jan Willem Dankbaar3, Tom J. Snijders4, Pierre A.J. Robe4, Joost J.C. Verhoeff1
1University Medical Center Utrecht, Radiation Oncology, Utrecht, The Netherlands; 2University Medical Center Utrecht, Medical Oncology, Utrecht, The Netherlands; 3University Medical Center Utrecht, Radiology, Utrecht, The Netherlands; 4University Medical Center Utrecht, Neurology and Neurosurgery, Utrecht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Treatment
of diffuse gliomas typically consists of surgical resection and subsequent
radiotherapy and/or chemotherapy. High-dose radiation can however lead to new
enhancing lesions on follow-up scans, which are challenging to distinguish from
tumor progression. These post-radiation lesions, including pseudoprogression
and radiation necrosis, occur in 20-30% of glioma patients and are thought to
stem from cerebral inflammatory responses and structural changes in the
cerebral vasculature. As development of these lesions might relate to the
effectivity of the treatment, we have investigated the association between
post-radiation lesions and overall survival (OS) in patients with diffuse
glioma.
Material and Methods
We
accessed a retrospective database of 144 adult cases with WHO grade II-IV
supratentorial gliomas, who received surgery and postoperative MRI within 3
days, and identified 65 patients who received radiotherapy after first surgery and
had subsequent MRI follow-up of at least 6 months. Patient follow-up was up to
60 months after start of radiotherapy. Post-radiation injury was defined as a
new enhancing lesion on CE-T1 MRI that stabilized or decreased after a minimum
of 3 months follow-up (Figure 1). OS was analyzed in a Cox-regression model, consisting
of development of post-radiation lesions, age, WHO grade, prescribed dose and
concurrent or additional chemotherapeutic treatment.
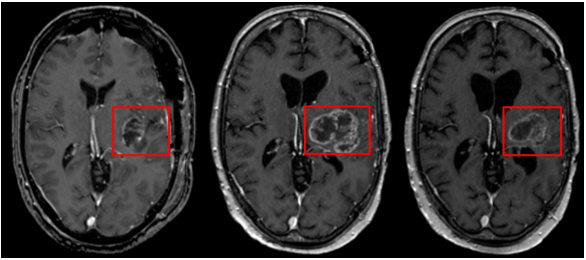
Figure 1. Patient with post-operative CE-T1 scan
(left), onset of post-radiation lesion (middle) and stabilization after 6
months (right).
Results
Post-radiation
injury occurred in 26 patients (36%) and had a median volume of 9.9cc.
Development of post-radiation lesions was significantly associated with a hazard
ratio (HR) of 0.538 [95% confidence interval (CI) 0.296 – 0.977] (Table 1) and these
patients had a longer median OS (25 months [95% confidence interval (CI) 20.0-30.0]
versus 16 months [95% CI 10.8-21.2]). Factors significantly associated with OS
were: 1) WHO grade 4 (compared to WHO grade 2), 2) prescribed dose of 60Gy and 3)
chemotherapeutic treatment (Table 1). Among patients with post-radiation
injury, lesion volume was not associated with OS
Table 1. Multivariable analysis for OS in diffuse glioma.
| Variable | Hazard Ratio (HR)
| 95%
Confidence Interval | P-value |
Post-radiation lesions
| 0.538
| 0.296
– 0.977 | 0.042 |
| Age | 1.016 | 0.986
– 1.047 | 0.297 |
WHO Grade - III vs II
- IV vs II
|
1.097 8.315 |
0.204 – 5.902
1.309 – 52.818 |
0.914
0.025 |
| 60 Gy
prescribed dose | 9.073 | 1.782
– 46.196 | 0.008 |
| Chemotherapy | 0.164 | 0.057
– 0.479 | 0.001 |
Conclusion
We
have investigated the relation between development of post-radiation lesions
and OS. Despite the therapeutic impasse these lesions often impose, we found
them to be a favorable prognostic factor, even after correcting for
predisposing factors. This finding could elude that post-radiation lesions
represent an effective treatment of diffuse glioma. Future prospective studies with larger sample
sizes should validate this finding.