Development of mid-treatment biological image guided adaptive radiotherapy (BIGART) for glioblastoma
Meetakshi Gupta,
United Kingdom
PD-0240
Abstract
Development of mid-treatment biological image guided adaptive radiotherapy (BIGART) for glioblastoma
Authors: Meetakshi Gupta1, Laura Mancini2, Sotirios Bisdas2, Spyros Manolopoulos3, Michael Kosmin1
1University College London Hospitals NHS Foundation Trust, Department of Radiotherapy, London, United Kingdom; 2National Hospital for Neurology and Neurosurgery, University College London Hospitals NHS Foundation Trust, Lysholm Department of Neuroradiology, Neuroradiological Academic Unit, Department of Brain Repair and Rehabilitation, IoN, UCL, London, United Kingdom; 3University College London, Department of Physics and Bioengineering, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Glioblastoma is a highly aggressive brain malignancy with dismal clinical outcomes. Multiparametric MR imaging (mpMRI) enables exploration of anatomical, biological and metabolic characteristics of tumours and their microenvironment, using techniques such as diffusion weighted imaging (DWI), chemical exchange saturation transfer (CEST), perfusion and spectroscopy.
Our work investigates mpMRI changes that occur during a course of standard chemoradiotherapy for glioblastoma, and the utilisation of biological imaging guided adaptive RT (BIGART) for treatment personalisation. We provide information on the development of these methodologies and a proof-of-principle case.
Material and Methods
Patients with newly diagnosed glioblastoma with residual tumour post-surgery who were planned for long course chemo-RT (60Gy/30# over 6 weeks with concurrent temozolomide as per Stupp protocol) were recruited to the study. They underwent mpMRI <7 days before starting RT and after 10, 20 and 30 fractions of RT.
Imaging was performed with 3T Magnetom Prisma (Siemens Healthineers, Erlangen, Germany). Neuroradiologist (SB) defined ROI on the mid-RT imaging, identifying areas of potential treatment resistance. These were used to create a biological target volume (BTV) as a mask registered to anatomical T1 weighted sequence. This was then co-registered within Eclipse to the original planning CT for adaptive treatment planning.
In our test case, we investigated the feasibility of escalating dose to the BTV from fraction 16 onwards via a simultaneous integrated boost (SIB) of 45Gy/15# (total BTV dose 75Gy/30#). The remainder of the PTV outside the BTV was planned to continue to receive 2Gy/fraction (total 60Gy/30#). Separate photon and proton plans were generated for this BIGART, keeping doses to organs at risk within standard clinical tolerances.
Results
Four patients were recruited in the study at the time of this analysis and a total of 14 mpMRI scans were performed. Changes were evident on mpMRI after 10 fractions that enabled BTV generation (Figure 1). The data framework to transfer the information from the non-anatomical mpMRI sequences to an ROI within the T1 weighted sequence has been shown to function, along with the co-registration of these ROIs within Eclipse.
We were able to successfully generate both photon and proton adaptive plans for these patients while keeping the biologically equivalent doses to OARs same as the routine 60Gy plans (Fig 2).
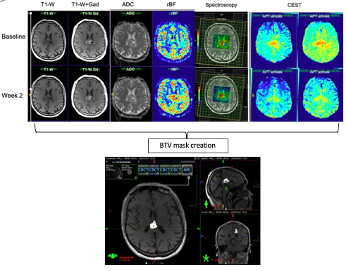
Fig1– Changes in mpMRI from baseline to Week 2 and creation of BTV mask
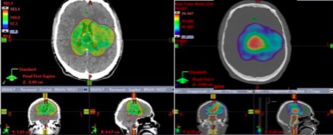
Fig2- Standard 60Gy photon plan (left) and 75Gy SIB proton plan (right) showing dose wash >57Gy
Conclusion
Multiparametric MRI changes are evident early during chemoRT for glioblastoma, and continue to develop throughout treatment. Personalisation of treatment adaptation using BIGART techniques appears feasible in this group of patients and warrants further investigation. Additional recruitment to our prospective mpMRI study will further our understanding and enable to refine our techniques.