Radiotherapy dose escalation in glioblastoma in the era of functional imaging: A prospective study
PD-0239
Abstract
Radiotherapy dose escalation in glioblastoma in the era of functional imaging: A prospective study
Authors: Renu Madan1, Chinnababu draksham1, Narendra Kumar1, Gaurav Trivedi1, Arun K Yadav1, Manjul Tripathi2, Shikha Goyal1, Divya Khosla1, Rajendra Basher3, Chirag K Ahuja4
1Postgraduate Institute of Medical Education and Research, Radiotherapy and Oncology, Chandigarh, India; 2Postgraduate Institute of Medical Education and Research, Neurosurgery, Chandigarh, India; 3Postgraduate Institute of Medical Education and Research, Nuclear medicine, Chandigarh, India; 4Postgraduate Institute of Medical Education and Research, Radiodiagnosis and Imaging, Chandigarh, India
Show Affiliations
Hide Affiliations
Purpose or Objective
Local failure
remains the major concern in glioblastoma (GBM) despite aggressive treatment. Pilot
studies have shown that escalated radiotherapy (RT) dose beyond 60 Gy improves outcome in GBM, although
the conclusive data is lacking. Here we present our preliminary data of RT dose
escalation using pentixafor PET scan. High 68Ga-pentixafor uptake is seen in glioma patients
expressing chemokine receptor-4 which helps in sharp demarcation between normal
brain and glioma cells.
Material and Methods
The prospective study was conducted over
a period of 18 months from March 2018 to December 2019. Post-operatively,
all GBM
patients underwent MRI brain and pentixafor PET scan. A delayed
contrast enhanced planning CT scan was co-registered with MRI and PET. RT was planned
in 2
phases.
Phase 1 GTV (GTV1) comprised of T2/flair abnormality,
PET avid
disease and post-op cavity. A margin of 2 cm was given to GTV1 for
phase 1 CTV (CTV1), which was expanded for 0.5 cm to generate phase 1 PTV
(PTV1). RT
dose of 46Gy/23# was prescribed to PTV1. Phase 2 GTV (GTV2) consisted of CT/MRI
contrast enhancing lesion, PET avid disease and post op cavity. A
margin of 2 cm was given to GTV2 to create phase 2 CTV (CTV2)
which
was expanded 0.5 cm to create phase 2 PTV (PTV2). RT dose of 14 Gy/7# was prescribed to PTV2.
PET avid disease was demarcated as GTV PET and a margin of 3mm was given to generate PTV
PET. PTV
PET received escalated RT dose 21 Gy/7# using simultaneous integrated boost in phase 2 (Total dose 67
Gy/30 #).
All patients received RT by VMAT along with concurrent and adjuvant TMZ. Following RT, patients who were lost to follow
up, were contacted telephonically. The data was prospectively maintained in Microsoft
Excel sheet. SPSS v 23 was used for statistical analysis.
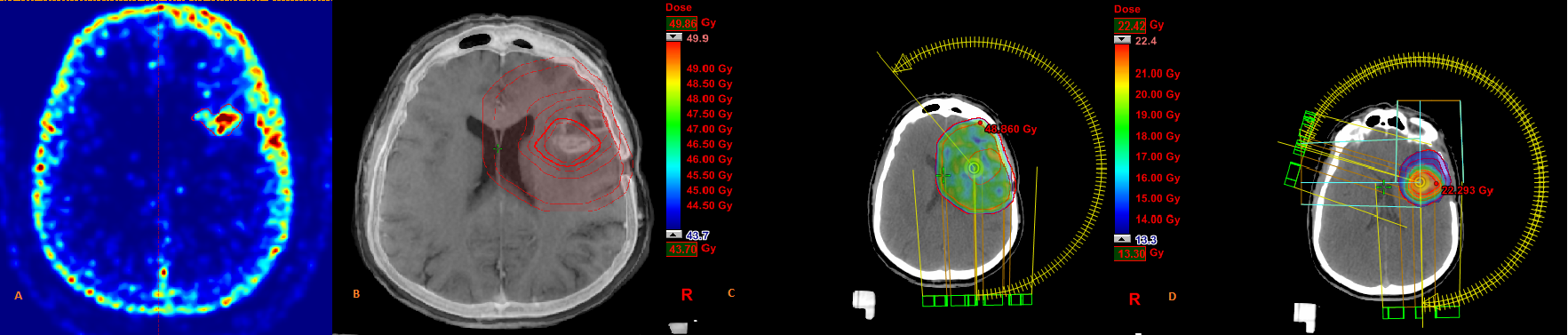
Figure 1 is showing (A)
Pentixafor PET showing metabolically active disease; (B) Target
volume delineation ; (C) Phase 1 dose colour wash; (D) Phase 2 dose colour wash including SIB
Results
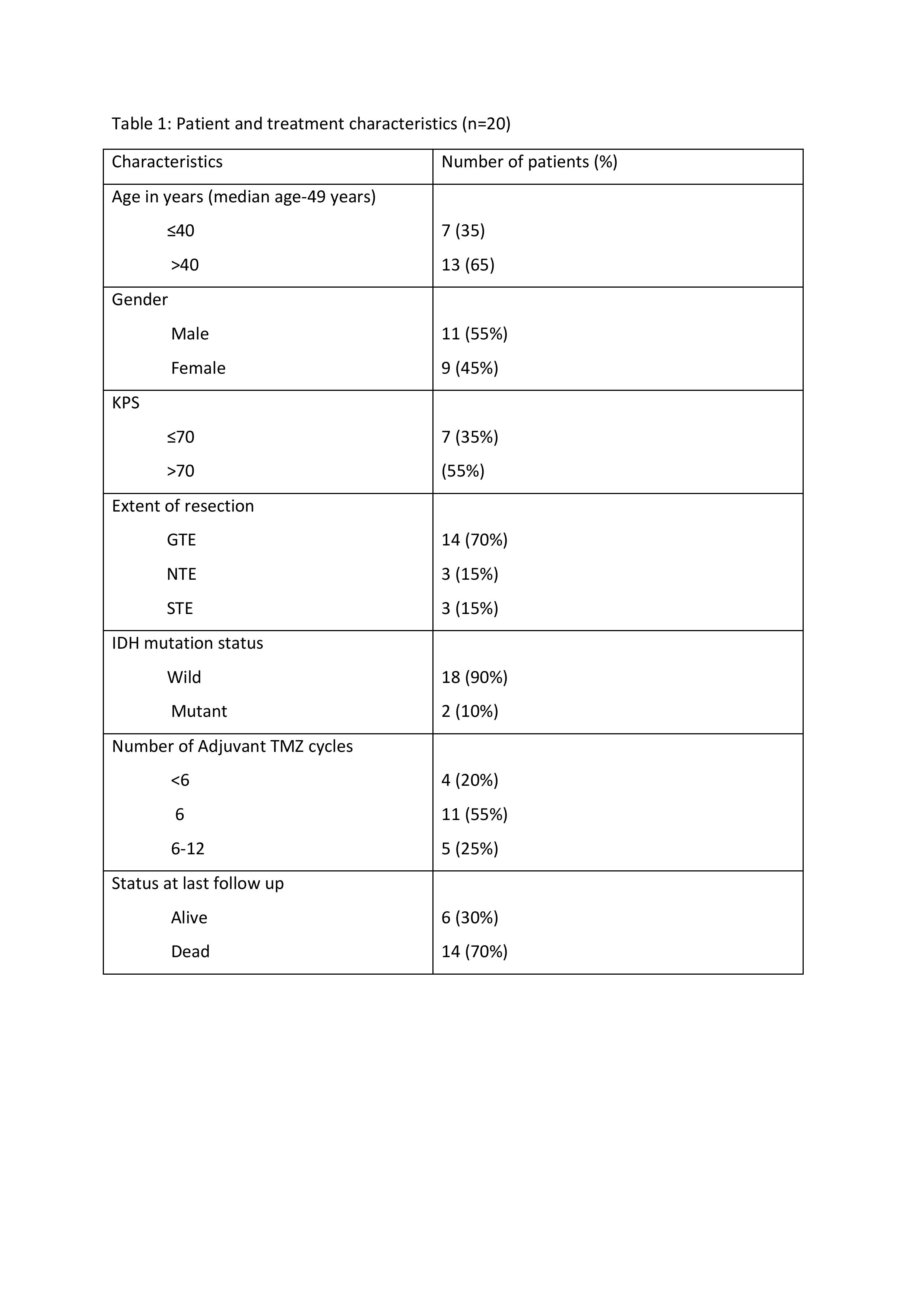
A total of 20 patients were analysed.
Patient and treatment characteristics have been shown in table 1. Median
follow up
was 23
months (20.8 ± 7.97). Fourteen patients had documented recurrence
and succumbed to the disease. A median overall survival (OS) of 23
months (95% CI, 17.15-28.8) was observed with estimated 1, 2 and 3 years OS
of
80%, 43.7% and 0% respectively. A significant association of
OS was
seen with extent of surgery (0.04). A non-significant trend towards
increased OS was seen in those with KPS >70, age <40 years and >6
cycles of TMZ. No patient developed symptomatic
radiation
necrosis.
Conclusion
Although radiotherapy dose escalation remains challenging in GBM, latest
technologies can help in targeting the metabolically active tumor with
higher dose without increasing the risk of radiation
necrosis. The
index study shows slightly higher median OS as compared to the historical data
indicating that radiotherapy dose escalation is feasible and
well tolerable in GBM patients and should be further
explored in the randomised trials.