Breathing amplitude is reduced by rapid shallow breathing at 60 breaths/minute
Zdenko van Kesteren,
The Netherlands
PD-0233
Abstract
Breathing amplitude is reduced by rapid shallow breathing at 60 breaths/minute
Authors: Zdenko van Kesteren1, Jeffrey Veldman1, Michael Parkes1, Geertjan Tienhoven1, Joost van den Aardweg2, Markus Stevens3, Arjan Bel1, Irma van Dijk1
1Amsterdam UMC, Radiotherapy, Amsterdam, The Netherlands; 2Amsterdam UMC, Pulmonology, Amsterdam, The Netherlands; 3Amsterdam UMC, Anesthesiology, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiotherapy in the thoracic-abdominal region, requires
generous margins to ensure tumor coverage due to respiratory motion, at the
expense of healthy tissue dose. We
investigated the influence of high frequency mechanical ventilation at 60
breaths/minute (brpm), with positive end expiratory pressure (PEEP) and without
percussion, on diaphragm motion amplitude using magnetic resonance imaging
(MRI).
Material and Methods
After
two training sessions, six healthy volunteers were scanned at a 3T MRI during
free breathing (FB) and during mechanical ventilation at 60 brpm without PEEP
and with 5, 10 and 15 cm H2O PEEP. In one sagittal plane of the right lung,
three minute cine-MRIs were acquired consisting of 350 2D images with a rate of
0.51 s/frame. The diaphragm motion amplitude was measured at a fixed point on
the right diaphragm. The median sagittal lung surface was calculated on these
350 sagittal images per volunteer. Significance of the differences were
determined by a Wilcoxon signed rank test (with the Bonferroni correction applied).
Results
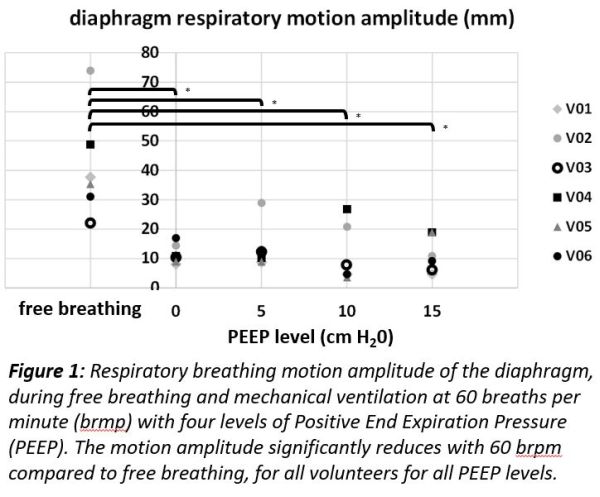
Mechanical
ventilation with 60 brpm and several levels of PEEP was easily adopted and well
tolerated by volunteers. Compared to FB, the median (range) diaphragm motion
amplitude of all volunteers significantly reduced by 76% (46% - 79%) from 37 (22
– 74) mm to 11 (8 – 17) mm during mechanical ventilation at 60 brpm without
PEEP (α=0.013;
p=0.008). The reduction was present for each volunteer and for all of the four
levels of PEEP (Fig 1). We could not establish a significant further reduction
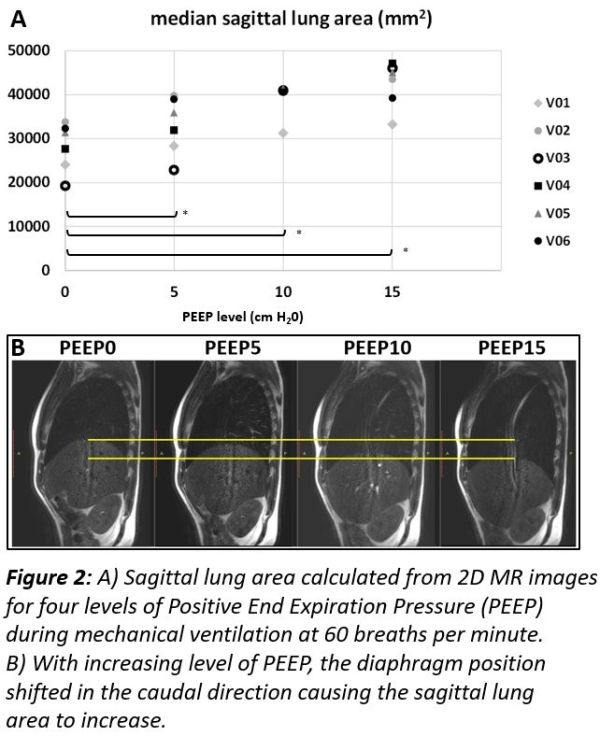
in motion amplitude for the various levels of PEEP. However, applying higher
levels of PEEP moved the diaphragm in a more caudal position resulting in an significantly
increased median lung area (Fig 2) of 18% for PEEP5, 31% for PEEP10 and 41% for
PEEP15, compared to no PEEP (α=0.017;
p<0.001).
Conclusion
Compared
to free breathing, mechanical ventilation at 60brpm without PEEP significantly reduced
the median diaphragm motion amplitude. Increasing PEEP did not further reduce the
motion. However, applying higher PEEP significantly increased the lung surface
measured on 2D images compared to no PEEP. Since increased lung volume is
associated with lower mean lung dose and a lower diaphragm position, altering
the position of the heart, applying high pressure PEEP during radiotherapy may
reduce toxicity even further.