Lung function after total body irradiation in myeloablative allogeneic stem cell transplantation
PD-0171
Abstract
Lung function after total body irradiation in myeloablative allogeneic stem cell transplantation
Authors: Xiaodan Wang1, Jann Mortensen2, Henrik Sengeloev3, Flemming Kjaer-Kristoffersen4, Peter Meidahl Petersen5, Lena Specht5
1National Cancer Center, Chinese Academy of Medical Science, Cancer Institute and Hospital, Beijing, China; 2Rigshospitalet, University of Copenhagen, Dept. of Clinical Physiology & Nuclear Medicine, Copenhagen, Denmark; 3Rigshospitalet, University of Copenhagen, Dept. of Haematology, Copenhagen, Denmark; 4Rigshospitalet, University of Copenhagen, Dept. of Oncology, Section of Radiotherapy, Copenhagen, Denmark; 5Rigshospitalet, University of Copenhagen, Dept. of Oncology, Copenhagen, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
To examine the
effect on lung function of technique and fractionation of total body
irradiation (TBI) in conditioning for myeloablative allogeneic stem cell
transplantation (allo-HSCT).
Material and Methods
From 09.2010 to
06.2019 178 patients with acute leukemia had TBI for allo-HSCT. 19 children and
37 pts. without lung function test (LFT) before TBI were excluded. The
remaining 122 pts. were divided into three groups treated in consecutive time
periods: 22 pts. in Group 1 were treated with 2D technology to a total dose of
11.3 Gy in 3 daily fractions; 49 pts. in Group 2 were treated with 2D
technology to a total dose of 12.0 Gy in 6 fractions in 3 days; 51 pts. in
Group 3 were treated with 3D technology (step-and-shoot) to a total dose of
12.0 Gy in 6 fractions over 3 days. Both techniques were delivered at extended
distance (3.5 – 4.2 m) and with a low dose-rate (0.08 - 0.125 Gy/min). Chemotherapy
conditioning was cyclophosphamide 120 mg/kg (TBI-Cy) for myeloid diseases and
etopophos (etoposide phosphate) 1800 mg/m2 (TBI-Eto) for lymphoid diseases. No
other changes expected to influence LFTs were made to the treatment during that
period. Pts. were to have spirometry and hemoglobin corrected diffusion
capacity (DLCO) before and 3, 6, and 12 months after TBI. We analyzed pts. with
complete data on LFTs before and at 6 and 12 months. Differences between groups
were compared by χ2 test.
Results
13, 29, and 31 pts
could be analyzed in Group 1, 2, and 3, respectively. There was no significant
difference in overall survival between the three groups. Forced vital capacity
and forced expiratory volume in the first second showed only insignificant
changes at the three timepoints. However, the DLCO declined significantly from
before to 12 months after TBI for Group 1, with no indication of recovery, see
Figure. The DLCO for Group 2 declined but recovered after 6 months, although
still not completely after 12 months, indicating that the finer fractionation
led to less lung damage. The DLCO for Group 3 declined less and recovered
completely, although compared to Group 2, the difference was not statistically
significant, indicating that the 3D technique with a dose variation of ≤10 %
achieved possibly even better sparing of the lung function.
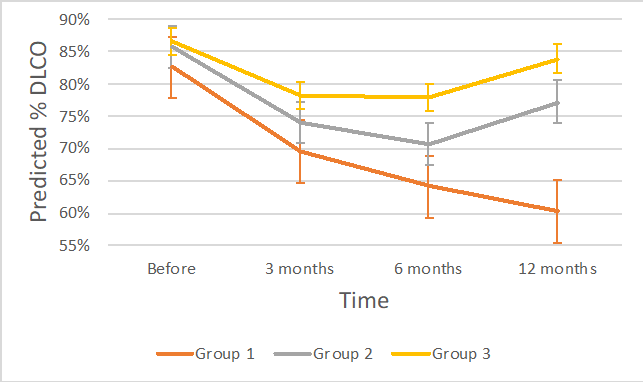
DLCO for the 73
patients with DLCO before, and 6 and 12 months after TBI
Conclusion
TBI in small fractions and planned with modern
3D techniques was associated with better sparing of lung function in pts.
treated with allo-HSCT.