Breath-hold proton therapy for mediastinal lymphomas: the expected effect on cardiac toxicity
Richard Canters,
The Netherlands
PD-0170
Abstract
Breath-hold proton therapy for mediastinal lymphomas: the expected effect on cardiac toxicity
Authors: Maaike Berbee1,1, Femke Vaassen2, Maud Cobben1, Kim Klugt van der3, Indra Lubken1,1, Bastiaan Ta1, Lars Murrer1, Richard Canters1
1Maastro, Radiation Oncology, Maastricht, The Netherlands; 2Maastro, Radiation Oncology, Maasticht, The Netherlands; 3Maastro, Radiation Oncoloy, Maastricht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Currently, at our clinic, patients with a limited stage mediastinal
lymphoma are either being treated with a photon technique in breath-hold (BH) or
a proton technique in free-breathing (FB). To date, most of our patients are being
treated with a BH photon technique as these plans result in the lowest mean
heart dose (MHD). Combining BH and proton therapy may result in a further
reduction of the MHD. With this study we
aim to quantify the dosimetric advantages and the expected effect on the risk
of cardiac toxicity of BH proton therapy for mediastinal lymphomas. Moreover,
we assessed if our current BH method results in sufficiently stable breath holds.
Material and Methods
BH CT scans of 10 patients with a mediastinal Hodgkin’s lymphoma who
were previously treated with a VMAT photon technique (5mm PTV margin) were used
to generate 10 proton plans for the same target volume and prescription dose. A
robustness margin of 5 was used for proton planning. Per patient the MHD of the
proton plan was compared with the MHD of the existing photon plan. For each
patient a ΔNTCP for the life time risk of ≥ grade 4 acute coronary events was
calculated using an existing and validated model (LIPP borstkanker, NVRO, 2020).
Moreover, mean lung dose (MLD) and V5Gy of the bilateral lungs were compared
per patient.
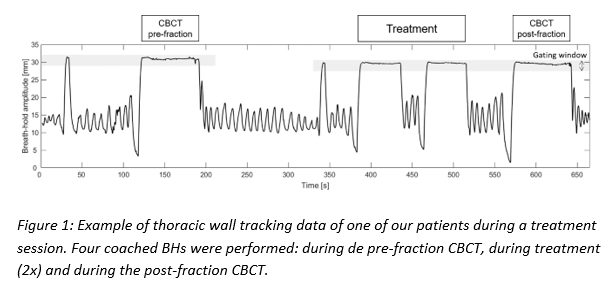
During the CT and photon fractions, the above-described patients
received visual BH coaching using a C-Rad Sentinel (during CT) and Catalyst (during
treatment) system with a gating window of 3 mm. BH stability of these 10
patients during photon treatment was evaluated using pre- and post-fraction (BH)
CBCT images and intra-fraction surface tracking data of the thoracic wall collected
using C-Rad (Figure 1).
Results
For all patients, proton planning resulted in a reduction of the MHD (Table
1). The median reduction was 2.2 Gy (IQR 1.5 Gy). As a consequence, using
proton therapy, the risk of ≥ grade 4 acute coronary events would be reduced in
all patients with a median ΔNTCP of 2.6% (IQR 2.5%). In 7 out of 10 patients
the ΔNTCP was ≥ 2%, the clinical threshold to qualify for proton therapy, while
in FB only 1 out of 10 patients qualified. Proton planning resulted in a
reduction of the MLD (median 2.5 Gy, IQR 1.6 Gy) and lung-V5Gy (median 18.7%, IQR
12.8%) in all patients.
CBCT analyses showed a CTV
intra-fraction movement of <4.5 mm in 90% of fractions. Surface tracking data showed an average intra-BH
variation of 1.5 mm and an average maximal inter-BH variation of 3.2 mm.

Conclusion
Our BH technique results in sufficiently
stable breath-holds for proton therapy. The BH proton technique resulted in a
lower MHD than the BH photon technique in all patients. In the current cohort,
BH proton therapy would have resulted in a clinically significant reduction of ≥
2% in the life time risk of ≥ grade 4 acute coronary events in the majority of
patients.