Non-parametric modelling and validation to identify pericardial regions predisposing risk of death
PD-0162
Abstract
Non-parametric modelling and validation to identify pericardial regions predisposing risk of death
Authors: MARIA THOR1, Jiening Zhu2, Aditya Apte1, Phong Tran1, Jung Hun Oh1, Annemarie Shepherd3, Andreas Rimner3, Allen R Tannenbaum4, Joseph O Deasy1
1Memorial Sloan Kettering Cancer Center, Medical Physics, NEW YORK, USA; 2Stony Brook University , Computer Science, NEW YORK, USA; 3Memorial Sloan Kettering Cancer Center, Radiation Oncology, NEW YORK, USA; 4Stony Brook University, Computer Science, NEW YORK, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
Cardio-pulmonary dose is a likely key cause for poor survival in locally-advanced non-small cell lung cancer (LA-NSCLC). Unlike preceding approaches which employ 1D or at most 2D dose metrics of pre-defined organs at risk (OARs), we incorporate unbalanced optimal mass transport (OMT) distance to dose distributions. This approach does not rely on either pre-definition of OARs or dose parameterization. The method ranks risk of death based on the OMT dose distance and was explored in the RTOG 0617 cohort, and validated in another large LA-NSCLC cohort.
Material and Methods
Dose and survival data for the RTOG 0617 cohort were retrieved from TCIA. Using a multi-step B spline algorithm, dose distributions were deformably registered to a reference patient with no mediastinal tumor involvement from the publicly available RIDER dataset, and the 398 patients with DSC>0.75 were retained for analysis. The unbalanced OMT distance was implemented via a vector-valued OMT approximation, measuring the dose spread pattern and total dose amount differences. OMT distances were translated into risk scores via the c-index. The validation cohort included 213 patients treated with radiotherapy to 45-66.6 Gy in 1.8-2 Gy fractions post-operatively. Risk of death in the validation cohort was measured as distances to the training reference patient. High-risk and low-risk anatomical regions were deduced from the agreement between the 50 riskiest (and least risky, respectively), patients above 60 Gy (0617 cohort) and above 50 Gy (validation cohort).
Results
In the RTOG 0617 cohort, the identified high-risk region subtracted the low-risk region was occupying the space between the descending aorta, left atrium, left and right pulmonary veins, pulmonary artery, and superior vena cava. The corresponding region in the validation cohort was in a similar but inferiorly located region.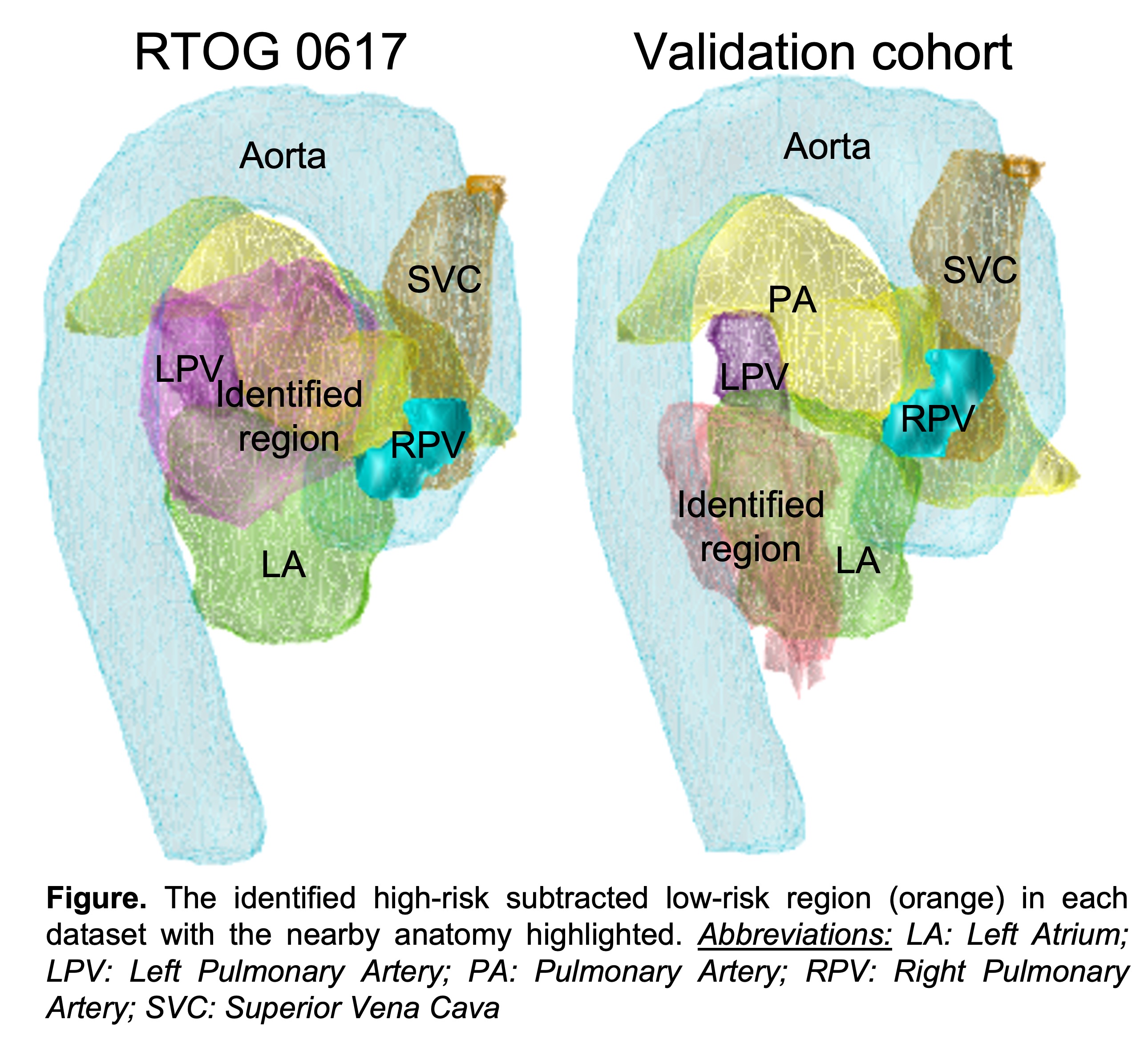
Conclusion
An unbalanced OMT approach was applied to identify dose distributions associated with high-risk and low-risk of death in two cohorts including the RTOG 0617 trial data. A similar but more inferiorly located region associated with high-risk of death was identified in the validation cohort. While there was no one-to-one correspondence between the identified region and already segmented structures in any of the cohorts, the regions are to some extent positioned nearby the atrioventricular node.