An objective measure of response on WBMRI in mHSPC treated with ADT, EBRT, and Radium-223
Valentina Giacometti,
United Kingdom
OC-0624
Abstract
An objective measure of response on WBMRI in mHSPC treated with ADT, EBRT, and Radium-223
Authors: VALENTINA GIACOMETTI1, Arthur C. Grey2, Aaron McCann3, Kevin M. Prise1, Alan R. Hounsell4,1, Conor K. McGarry4,1, Joe M. O’Sullivan5,1
1Queen's University Belfast, Patrick G. Johnston Centre for Cancer Research, Belfast, United Kingdom; 2Northern Ireland Cancer Centre, Belfast Health and Social Care Trust, Department of Imaging Services, Belfast, United Kingdom; 3Belfast Health and Social Care Trust, Radiological Sciences and Imaging Regional Medical Physics Service, Belfast, United Kingdom; 4Northern Ireland Cancer Centre, Belfast Health and Social Care Trust, Department of Radiotherapy Physics, Belfast, United Kingdom; 5Northern Ireland Cancer Centre, Belfast Health and Social Care Trust, Department of Clinical Oncology, Belfast, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Bone is the most common site of metastasis
in advanced prostate cancer. Assessment of response to therapy in bone metastases remains
challenging [1]. Magnetic resonance (MRI) plays an important
role in bone metastasis detection and response assessment. However, an objective
measure of response remains elusive. The aim of this
study was to generate an objective method to assess MRI response in the
vertebrae of patients with metastatic hormone sensitive prostate cancer (mHSPC),
before/after radiation therapy and Radium-223 and to correlate changes with clinical
outcomes, including survival.
Material and Methods
Whole body MRI (WBMRI) images from 25 patients from the neo-adjuvant
Androgen Deprivation Therapy pelvic Radiotherapy and RADium-223 clinical trial
(ADRRAD) [2] were imported into the Varian Eclipse (v13.5) (Varian Medical
Systems, Palo Alto) treatment planning system. Patients received androgen
deprivation therapy (ADT), and 6 cycles of Docetaxel prior to external beam radiotherapy
(EBRT) (74Gy/37 fractions to prostate and pelvic nodes), and 6 cycles of
Radium-223 (55kBq/kg). Three sets of WBMRI were
acquired: (MRI1) baseline scan performed at most 28 days before commencing EBRT,
(MRI2) performed at 2 months post completion of Radium-223 and (MRI3) performed
6 months post completion of Radium-223. MRI response was assessed by a
radiologist based on post baseline MRI images.
Vertebrae outside the EBRT field were semi-automatically contoured in the
sagittal T1 sequences of the three sets of WBMRI, and the MRI intensity was
measured. To compare the differences in intensity across MRI1, MR2 and
MRI3, spinal cord was chosen as a reference tissue to normalise the measurements.
The correlation between MRI intensity and clinical outcomes
was investigated by performing Mann-Whitney-Wilcoxon and Student’s t-test in R
(v4.1.0) (statistical significance set at p=0.05). Survival curves were
generated and discrimination measures for survival outcome were investigated for
MRI1.
Results
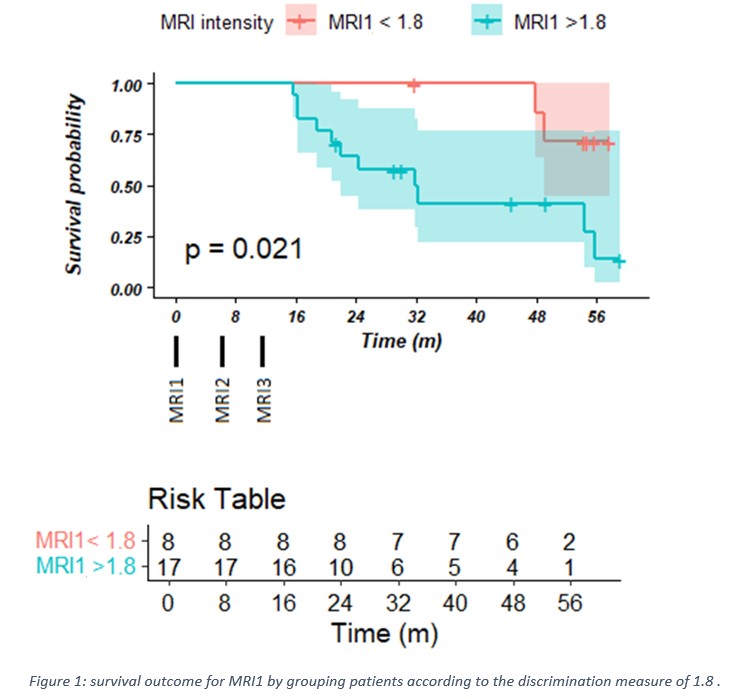
Using a discrimination measure
of 1.8 on the MRI1
normalised spine intensity, MRI1 was found to be a reliable
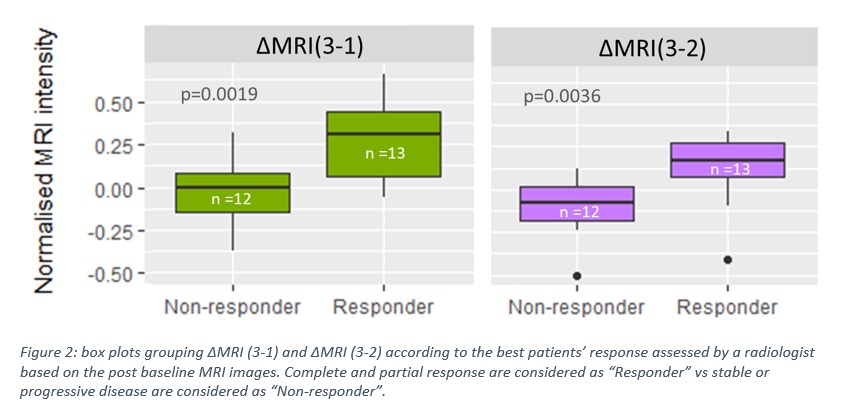
quantitative indicator (p=0.021) correlating with overall survival (Figure 1). ∆MRI(3-1)
and ∆MRI(3-2) were found to be reliable quantitative indicators
(p<0.05) for distinguishing responder
and non-responder patients (as defined by best response annotated independently
by a radiologist) (Figure 2). No significant
differences were found between patient
response vs MRI1 and ∆MRI(2-1).
Conclusion
We have identified a potentially useful objective measure of response on WBMRI
of vertebrae containing bone metastases in mHSPC which correlates with overall
survival and subjective radiological response. Further studies are needed to
validate our findings in a larger dataset.
References
[1] A. Turpin et al.,
Front. Oncol., 10 (55), 2020.
[2] Turner PG, et al., Clin
Cancer Res., 27(16), 2021.