Dosimetric Effects of Bladder Preparation and Its Impact on QoL for Ca Prostate SBRT Pts on MR-Linac
Sin Ting Chiu,
Hong Kong (SAR) China
MO-0308
Abstract
Dosimetric Effects of Bladder Preparation and Its Impact on QoL for Ca Prostate SBRT Pts on MR-Linac
Authors: Sin Ting Chiu1, Man Chun Lee1, Yuen Yan Chan1
1Hong Kong Sanatorium & Hospital, Department of Radiotherapy, Hong Kong, Hong Kong (SAR) China
Show Affiliations
Hide Affiliations
Purpose or Objective
MR-Linac (MRL) allows daily adaptive treatment (Tx) plan according to the change of contour and position. Patient undergoes SBRT prostate in MRL thus needs to tolerate the urgency of full bladder for a longer treatment time. An appropriate protocol of bladder control is needed to avoid patient void during a longer Tx time as well as to minimize the effect of bladder filling on the variation of bladder dose and prostate shape intra-fractionally. This retrospective study aims to evaluate the local practice on bladder control, which proceeds treatment with a pre-treatment (Pre-Tx) ultrasound-based measurement of 80% of CT reference volume at around 120ml, is appropriate and reproducible.
Material and Methods
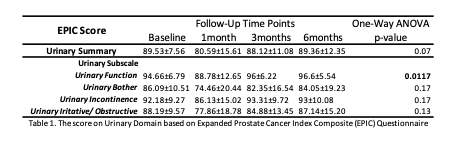
30 prostate cancer patients underwent SBRT in MRL, were recruited retrospectively. The delineated bladder from T2 weighted MRIs acquired across 3 time points (pre, intra and post Tx) were compared statistically in terms of its filling volume, centroid displacement, volumetric overlap using Dice similarity coefficient (DSC) and dosimetry distribution. Its impact on patient quality of life was assessed by comparing the Expanded Prostate Cancer Index Composite (EPIC) score on urinary domain across 3 time points (pre, post 1mth and post 3 mth Tx).
Results
A total of 450 MRI scans from 30 patients were compared and analyzed. The bladder volume increased significantly (p<0.0001) from a pre-Tx mean of 111.1ml ± 26.1, to 140.4ml ± 35.9, intermediately at a filling rate 1.22ml/min and 170.1ml ± 44.3 after Tx at a filling rate 1.39ml/min.
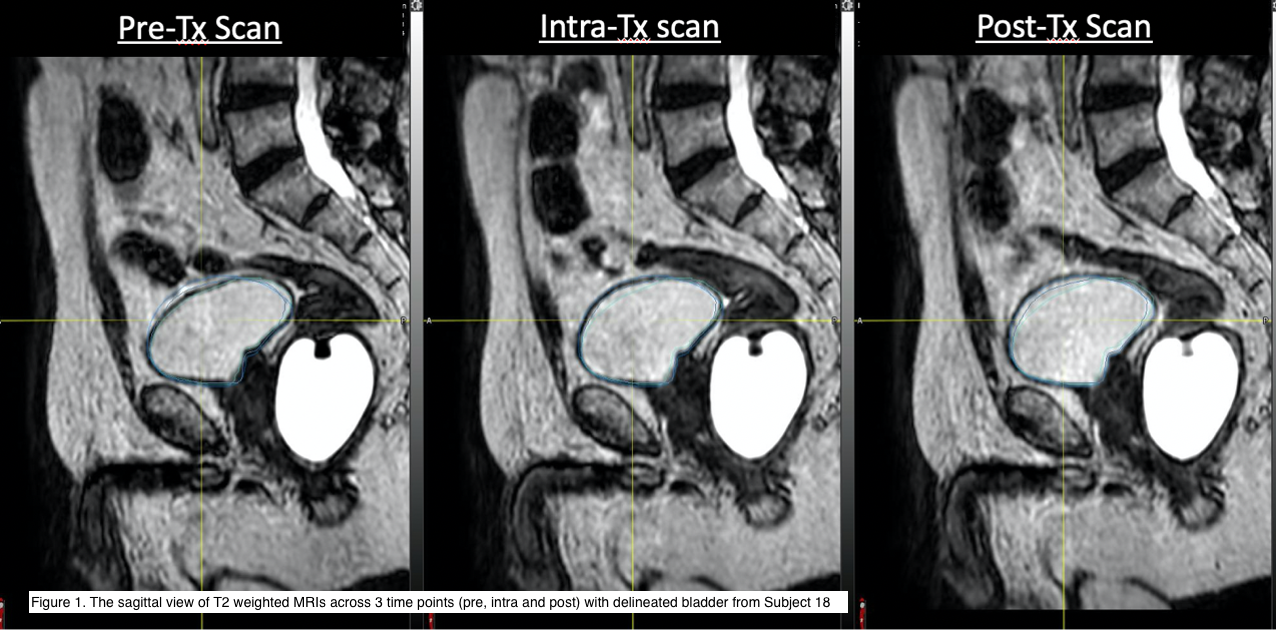
The increased bladder didn’t affect significantly x-axis of the centroid (p=0.07), but y axis and z axis (p<0.0001), which were a significant 0.7mm shift to right and 2.2 mm shift to the anterior between pre and intra scan; a significant 2.2 cm mm shift to the anterior and a 0.8mm shift to the left (p=0.0046) between the intra and post scan were found. The mean DSC was 0.9 between pre and intra scan and 0.8 between pre and post scan. For the bladder dose, there is no significant difference on Vtarget dose=41.6 (p=0.2), V38 (p=0.2) and V36 (p=0.1). However, a significant decrease of 2% on V20 (p<0.0001) and 0.9Gy on Dmean (p<0.0001) was found between the pre and post scan. The mean EPIC score on urinary domain was 89.5 for pre-Tx, 80.6 for post 1 mth Tx, 88.1 for post 3 mth Tx and 89.4 for post 6 month.
Conclusion
The result showed the high dose zone to bladder was consistent as the daily adaptative treatment plan even the bladder volume was increased during the treatment. Despite the EPIC Score on urinary function shows significant difference, most of the urinary function returned to baseline level 3 months after treatment. Thus, this bladder preparation protocol was feasible and tolerable for patients undergoing prostate radiotherapy on MRL, which requires a longer treatment duration for online adaptive procedure.