No need for manual adjustments of deep learning segmentation in oropharyngeal cancer?
Hanne van de Glind,
The Netherlands
MO-0549
Abstract
No need for manual adjustments of deep learning segmentation in oropharyngeal cancer?
Authors: Hanne van de Glind1, Ilse G. van Bruggen2, Johannes A. Langendijk2, Stefan Both2, Charlotte L. Brouwer2
1Universitair Medisch Centrum Groningen , Department of Radiation Oncology, Groningen, The Netherlands; 2Universitair Medisch Centrum Groningen, Department of Radiation Oncology, Groningen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Delineation of organs at risk (OAR’s)
plays a critical role in radiotherapy treatment planning. However, the
segmentation of OAR’s can be very time-consuming, especially in the head and
neck region. The
accuracy of our deep learning based automated segmentation is currently within
interobserver variability, however the influence of its use in treatment
planning – without performing manual adjustments – is still unclear. We compared dose and normal tissue
complication probability (NTCP) of fully automated vs. adjusted deep learning contouring
(DLC) for volumetric modulated arc therapy (VMAT) and intensity-modulated
proton therapy (IMPT).
Material and Methods
A test set of 10 patients, who were
treated for oropharyngeal cancer between February 2021 and July 2021 in the
UMCG, was selected. The patients were treated with a prescribed dose of 70 Gy
in 35 fractions to the primary tumour and 54.25 Gy to the elective lymph node
areas. DLC (Mirada
Medical, Oxford, United Kingdom) was used for automated segmentation of OAR’s. Treatment
plans were created in RayStation Development 10B using internally validated
machine learning based automated planning models (RaySearch Laboratories, AB, Stockholm, Sweden). For every patient four plans were
created: DLC VMAT, DLC adjusted VMAT, DLC IMPT and DLC adjusted IMPT. The DLC
plan is optimized using automatically segmented DLC. The DLC adjusted plan is
optimized using manual adjusted DLC by a
radiation therapy technician and approved by a radiation oncologist. NTCP
values for the development of late xerostomia and dysphagia were calculated and
compared between the DLC and DLC adjusted plans. The input variables to the
NTCP model for xerostomia were the mean planned dose to the parotid and
submandibular glands, and for dysphagia the mean dose to the oral cavity and
pharyngeal constrictor muscles based on the DLC and DLC adjusted plans. All
dose and NTCP variables were derived using the manually adjusted contours.
Results
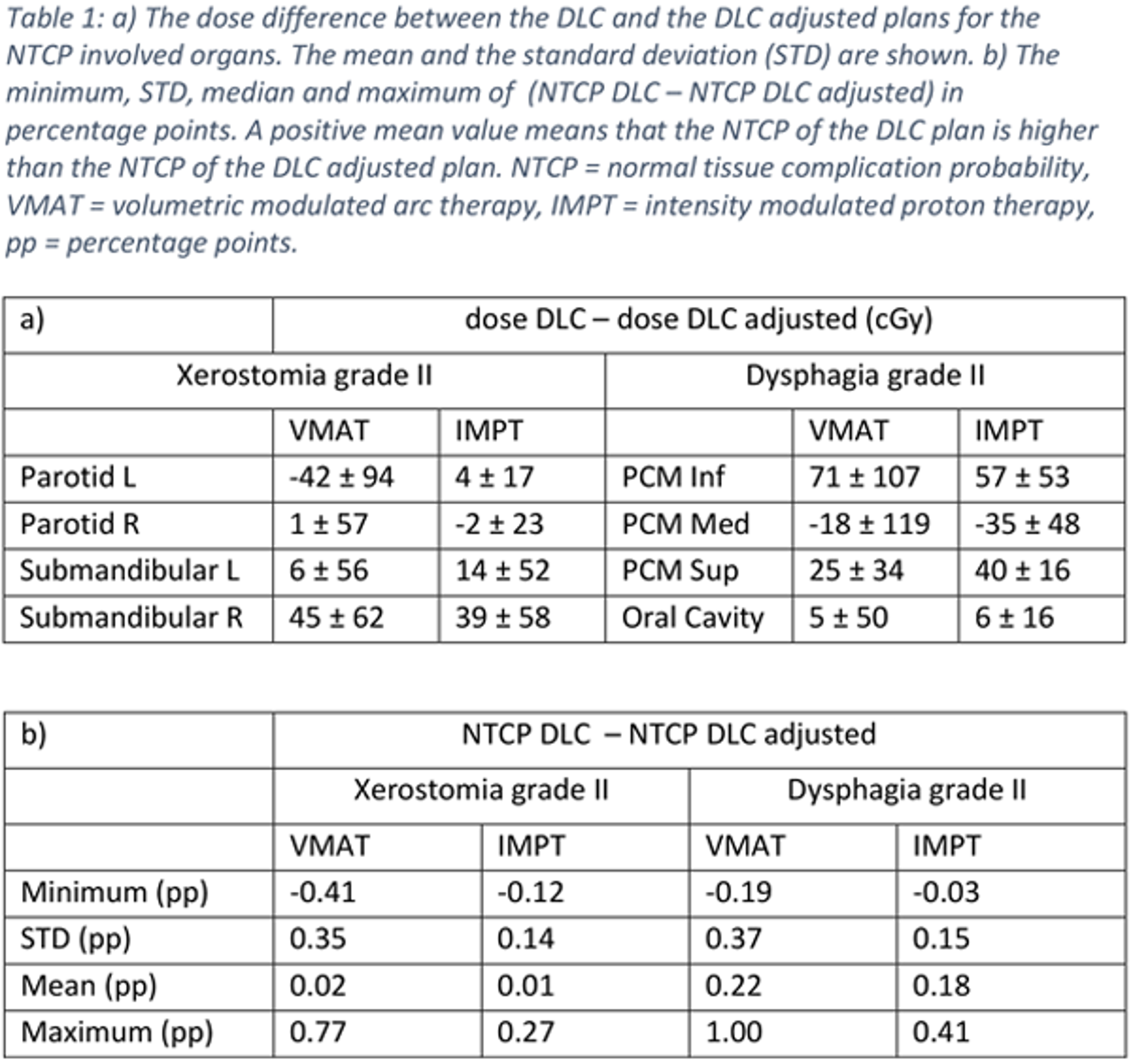
The mean dose differences between the
DLC and DLC adjusted plans for the OAR’s relevant for the NTCP’s were within 0.07
Gy (Table 1a). The mean difference in NTCP (NTCP DLC – NTCP DLC adjusted) was small:
-0.08 percentage point (pp) for VMAT and 0.11 pp for IMPT for xerostomia grade
II, and 0.16 pp for both VMAT and IMPT for dysphagia grade II (Table 1b). Statistically
significant difference was found between the NTCP of the DLC and DLC adjusted
IMPT plans for dysphagia (p = 0.01), as shown in Figure 1.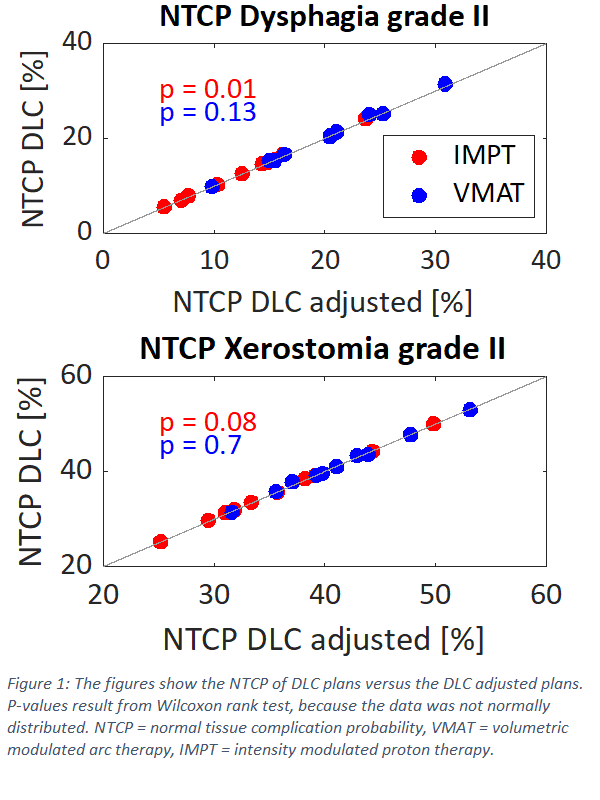
Conclusion
Mean OAR dose and NTCP values resulting
from VMAT and IMPT plans based on automated DLC are in agreement with VMAT and
IMPT plans based on manually adjusted DLC (mean dose deviations within 0.07 Gy,
NTCP within 1 pp). This suggests a limited effect of the manual adjustments
made to automatically segmented DLC for VMAT
and IMPT treatment of oropharyngeal cancer patients.