FLASH-dose and dose-rate calculations for 1x34Gy lung SBRT using proton transmission beams
MO-0543
Abstract
FLASH-dose and dose-rate calculations for 1x34Gy lung SBRT using proton transmission beams
Authors: Patricia van Marlen1, Wilko Verbakel1, Ben Slotman1, Max Dahele1
1Amsterdam University Medical Center, Radiation Oncology, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
The FLASH-effect, a
reduction in normal tissue toxicity with similar tumor control after ultra-high
dose-rate radiotherapy (UHDR-RT), requires not only high dose-rates, but
probably also a minimum dose delivered in a certain time period. The exact dose
threshold is unknown but could be in the range of 4-8Gy, which, if this is the
case, would limit the possible clinical applications. In addition, for scanning
proton beams, it is unclear how to define the dose-rate for the dose-rate threshold. In this work we
aimed to identify factors that might limit the ability to achieve the FLASH-effect
in a scenario attractive for UHDR-RT (high fractional beam dose, small target,
few OARs): single-fraction 34Gy lung SBRT.
Material and Methods
Clinical VMAT-plans, 3-field
IMPT-plans and 5-field UHDR transmission beam (TB) plans were compared for six
small and one large lung lesion. For the TB-plans the dose-rate was calculated
using four methods (Figure 1B): (1)
UHDR-contribution (UHDRc) is the percentage of dose delivered at spot dose-rates
higher than an UHDR-threshold, (2) dose-averaged dose-rate (DADR) is the average
dose-rate weighted by the dose contribution, (3) pencil-beam scanning dose-rate
(PBS-DR) considers a certain part of the dose and the time it takes to deliver
that dose and (4) the average dose-rate (ADR) divides the total dose of a field
by its total irradiation time. The
FLASH-percentage (percentage of dose delivered at dose-rates ≥40/100Gy/s and
≥4/8Gy) was determined for various variables: a minimum spot time (minST) of
0.5/2ms, maximum nozzle current (maxN) of 200/400nA and two gantry current (GC)
techniques (energy-layer based [EB]: GC is based on the lowest number of
monitor units within the energy-layer; spot-based [SB]: GC varies per spot).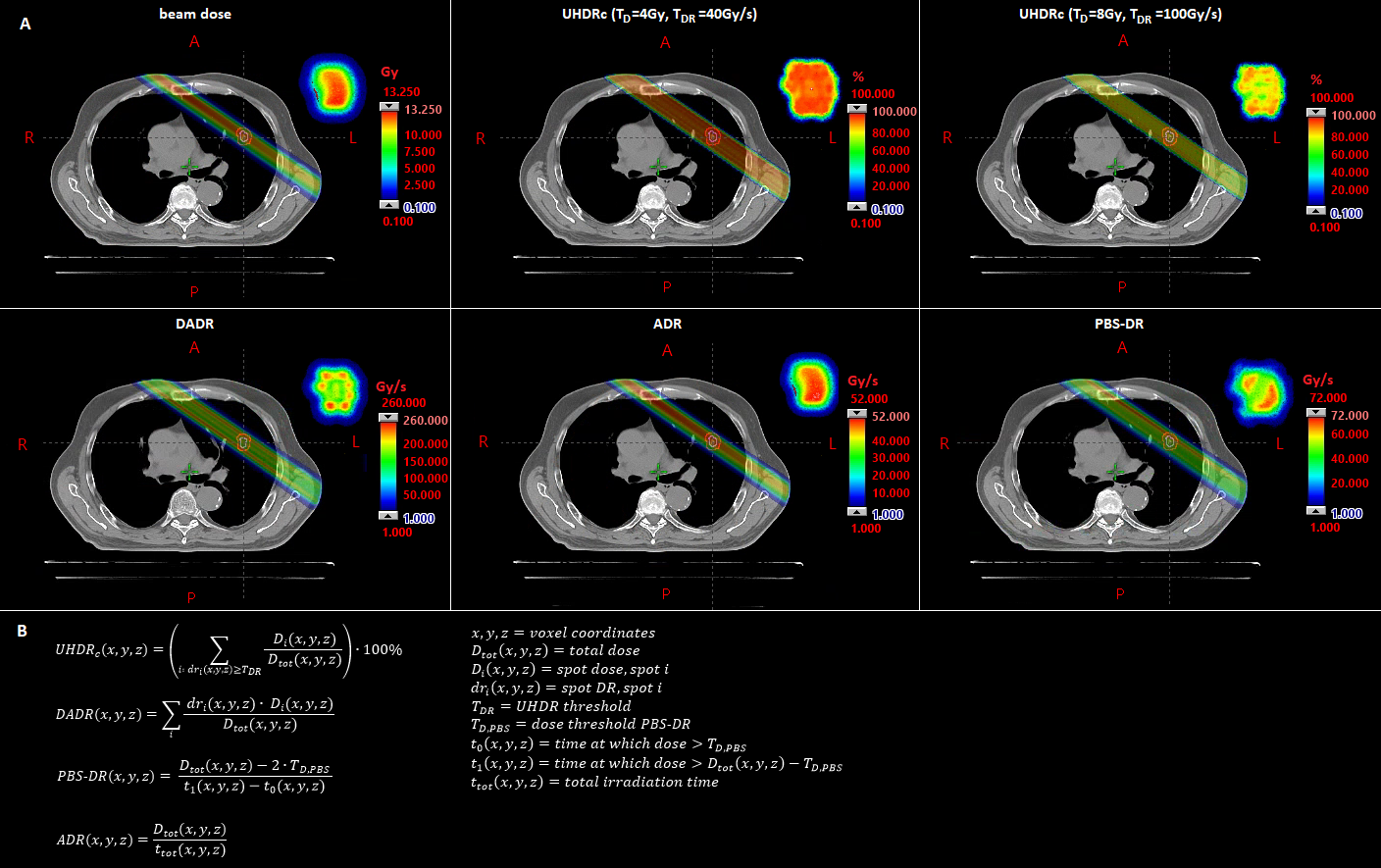
Results
Doses to OARs were
similar between TB and VMAT-plans, but TB-plans have higher rib, skin and
ipsilateral lung dose than IMPT, due to TB exit dose. Figure 1A shows the different dose-rates in a
single beam. Dose-rate calculation methods not considering scanning time (UHDRc,
DADR) achieve FLASH-percentages between ~30-80%, while methods considering
scanning (PBS-DR, ADR) often achieve <30% (Table 1). FLASH-percentages
increase for lower minST/higher maxN and when using SB GC instead of EB GC,
often approaching the percentage of dose
exceeding the dose threshold. For the
small lesions average TB beam irradiation times (including scanning) varied
between 0.06-0.31s and total irradiation times between 0.28-1.57s, for the
large lesion beam times were between 0.16-1.47s with total irradiation times of
1.09-5.89.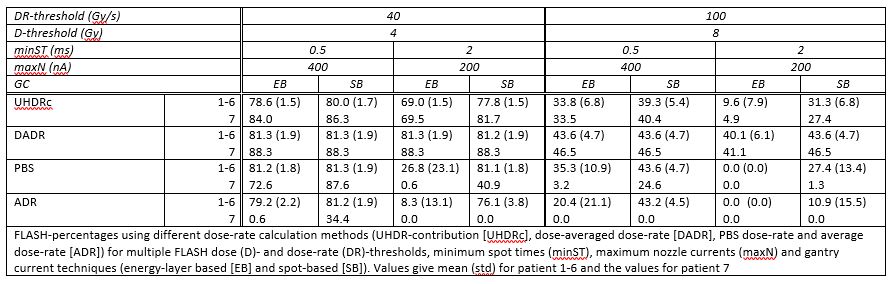
Conclusion
In a theoretically
advantageous scenario for FLASH we found that UHDR proton TB-plan dosimetry was
similar to VMAT, but inferior to IMPT, and that decreasing minST or using a SB
GC increase the estimated amount of FLASH. For the appropriate machine/delivery
parameters high enough dose-rates can be achieved regardless of calculation
method, meaning that a possible FLASH dose threshold could be the primary
limiting factor.