We
identified 256 eligible patients, and excluded 41 (no planning MRI) and 20 (no
follow-up MRI), resulting in a study population of 195 patients (table). Of
those 171 patients had radiologic progression. Progression was local-only in
56%, non-local in 15%, and combined in 16% of patients. Beyond first progression,
combined progression increased to 31%, non-local remained stable (15%), and
local-only decreased to 42%.
Median (95%
CI) time to progression/OS was 7.0 (5.8-8.2)/18.0 (15.1-20.9) months in the
local-only, 12.0 (10.9-13.2)/24.0 (16.3-31.7) in the non-local, and 7.0
(4.3-9.8)/12.0 (9.8-14.2) in the combined group, respectively.
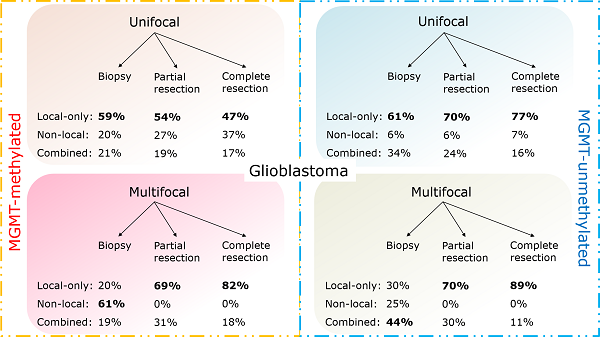
In multivariable analysis, MGMT-status
and EOS were significantly associated with type of progression (p-value 0.023
and 0.024, respectively). The obtained prediction model (AUC 0.71) contained
these variables and tumour focality as this was regarded as an important
potential confounder (figure). The probability of having local-only progression
varied between 20 and 89% for the respective subpopulations. All patients with
unifocal disease, and those with multifocal disease who had undergone a partial
or complete resection, had the highest probability of local-only progression, regardless
of MGMT-status.