Relationship between 4D CT quality and survival after lung cancer radiotherapy
MO-0389
Abstract
Relationship between 4D CT quality and survival after lung cancer radiotherapy
Authors: Marcel van Herk1, Gareth Price1, Eliana Vasquez Osorio1, Alan McWilliam1, Corinne Faivre-Finn1, Azadeh Abravan1
1University of Manchester, Division of Cancer Sciences, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Recently, Sentker et al reported that artifacts in 4DCT due
to irregular breathing and under-sampling are associated with local recurrence
in 62 lung and liver SABR patients (R&O 2020). This study suggested that
acquisition quality of 4DCT could have a measurable impact on treatment quality
and survival. The aim of this study is to investigate this finding in a large
cohort of lung cancer patients.
Material and Methods
For 991 lung cancer patients treated with conventional
radiotherapy between 2017 and 2020, DICOM objects of breathing traces were collected
from a pressure belt during 4DCT. In our clinical protocol, scans of slow
breathing patients can be too short to cover the entire lungs, because scan
time is limited at 120 s. In this case a free breathing scan is also taken. In-house
software was used to collect the total scan duration, average and standard
deviation (SD) of breathing period (using peak detection after Gaussian
smoothing), and average and SD of belt amplitude. Correlations between the
breathing trace parameters and clinical variables including age, tumour stage, performance
status (PS), comorbidity ACE score, and tumour volume were determined. Univariable
and multivariable Cox survival models were constructed with and without breathing
trace parameters.
Results
Visual inspection of a subset of scans showed moderate
artifacts in ~25% of scans, but very rarely at the tumour level. The average
breathing period was negatively associated with tumour volume (Wilcoxon test at
median period, p=0.003) and PS (p=0.02) but was strongly correlated with total
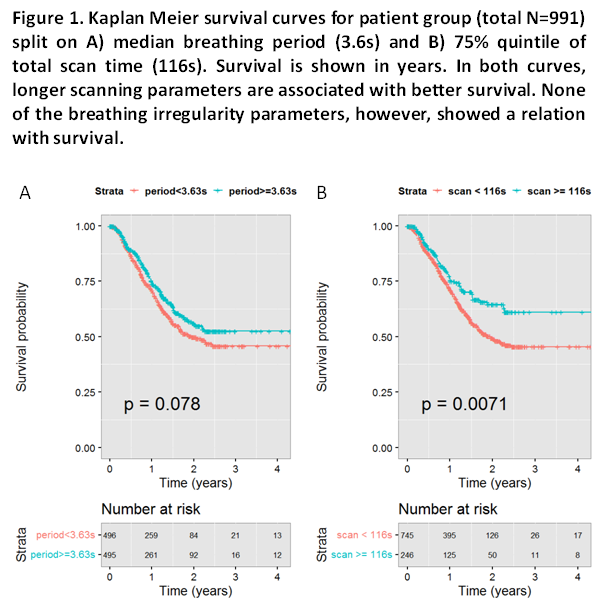
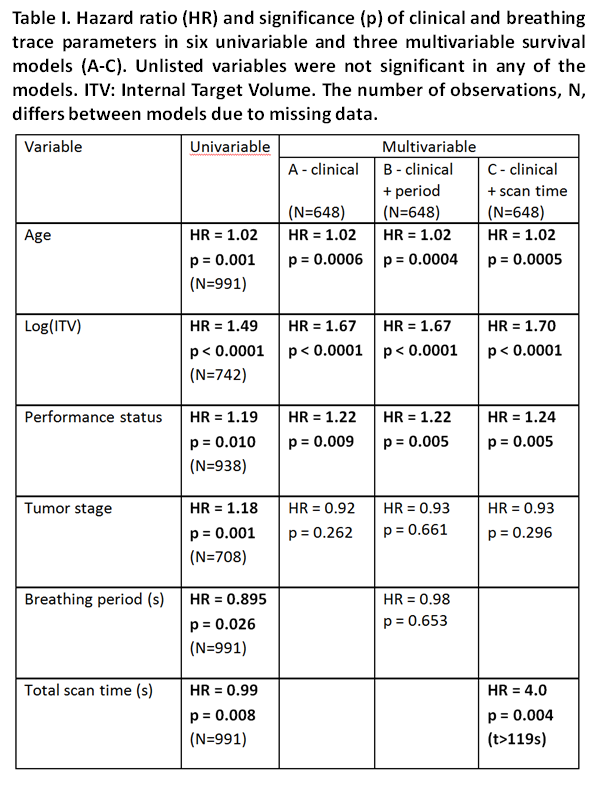
scan time (r=0.63). In univariable Cox analysis (Table I), a longer average
breathing period was associated with longer survival (HR=0.89 s-1,
p=0.026) as demonstrated in Fig 1a. Also, a longer scan time was associated
with longer survival, especially for scan times close to 120 s (Fig. 1b). None
of the parameters describing breathing irregularity, as proxy for 4DCT
artifacts, were associated with survival in univariable
analysis. In multivariable modeling (Table I), combining commonly used clinical
variables (A) with breathing period (B) did not improve the model. When combining clinical variables with total
scan time (C), total scan time > 119 s was significant for worse outcome (p=0.004).
Conclusion
This study did not find that 4DCT artifacts from breathing
irregularity are associated with poorer survival. Both longer scan times and
longer breathing periods were associated with survival, possibly because
patients with smaller tumours and better performance status tend to breathe slower.
This finding is opposite to Sentker, where longer periods caused under-sampling
artifacts, possibly because of differences in scan protocol. In multivariable
analysis the effect disappeared except for a negative effect of long scan times that may be related to missing information
when a full scan cannot be completed. Manufacturers should fix this.