Impact of operability and total metastatic ablation on outcomes after SABR for oligometastases
MO-0711
Abstract
Impact of operability and total metastatic ablation on outcomes after SABR for oligometastases
Authors: Shankar Siva1, Mathias Bressel2, Paolo Sogono1, Mark Shaw1, Sarat Chander1, Julie Chu1, Nikki Plumridge1, Keelan Byrne1, Gargi Kothari1, Nicholas Bucknell1, Nicholas Hardcastle3, Tomas Kron3, Greg Wheeler1, Michael MacManus1, Gerard G Hanna1, David L Ball1, Steven David1
1Peter MacCallum Cancer Centre, Department of Radiation Oncology, Melbourne, Australia; 2Peter MacCallum Cancer Centre, Centre for Biostatistics and Clinical Trials, Melbourne, Australia; 3Peter MacCallum Cancer Centre, Department of Physical Sciences, Melbourne, Australia
Show Affiliations
Hide Affiliations
Purpose or Objective
Operability status is prognostic for survival
after SABR in primary non-small cell lung cancer. Subtotal ablation of all
sites of oligometastases was negatively predictive of progression free survival
(PFS) in the ORIOLE phase II trial. This study aims to assess the prognostic
influence of operability and total metastatic ablation of all sites of
oligometastatic disease.
Material and Methods
Consecutive patients had operability status and
presence of subtotal versus total metastatic ablation recorded prospectively on
an institutional database. Data was retrospectively analysed with institutional
ethical approval. Inclusion criteria was 1-5 sites of active extracranial oligometastases.
The primary objective was to compare overall survival (OS) and PFS between
cohorts. Secondary objectives were to describe patterns of failure, high grade
treatment toxicity (CTCAE v4.0), and freedom from systemic therapy (FFST). Multivariable
Coxregression was performed to adjust for age, ECOG, Charlson Comorbidity
Index (CCI), synchronous vs. metachronous oligometastases and number of
metastasis at time of SABR.
Results
401 patients with 530 treated oligometastases
were included, with a median follow-up of 3 years. The median age was 67 years and
67% were male. Common histologies included prostate (24%), lung (18%),
gastrointestinal (19%) and breast (11%). The total number of metastases (currently
active and prior) was 1 in 47% of patients, 2-5 in 51%, and >5 in 2%.
Radical treatment to the primary was delivered in 96% of patients. Grade 3-4
toxicities were reported in 3% (n=14). Cumulative incidence at 5-years of local
only failure was 6%, local and distant was 2%, and distant only failure was
58%. The 3- and 5-year OS [95% CIs] were 68% [62-73] and 54% [47-61], and PFS
was 20% [15-25] and 14% [10-20]. The 3- and 5-year FFST [95% CIs] was 40%
[34-46] and 31% [24-37]. 76 patients were medically inoperable and 325 were
medically operable. Inoperable patients were older (median 73 vs 65 years), had
a higher CCI (median 10 vs 8) and poorer ECOG status (47% ECOG 0 vs 71%) than
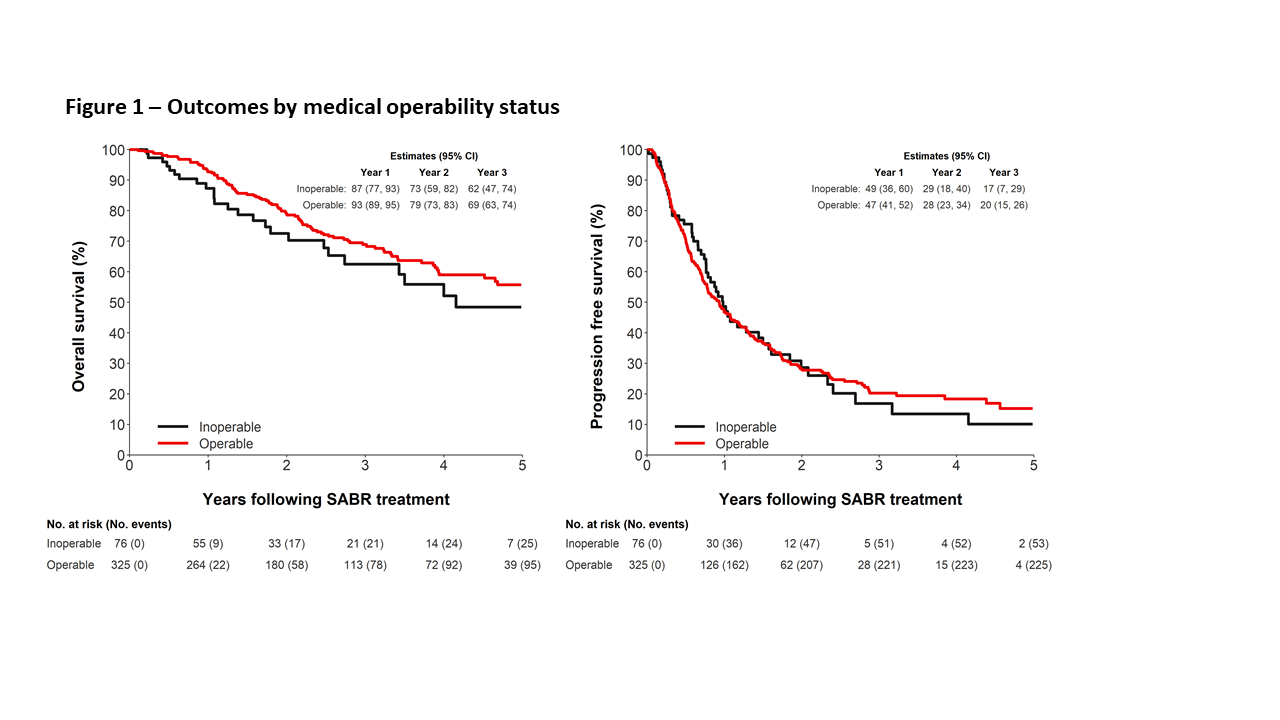
operable patients (all p-values <0.001). Operability status was not prognostic
for OS (logrank p=0.095) or for PFS (logrank p=0.9), (Figure 1). The
adjusted HR was 1.0 (95% CI: 0.6-1.7; p=0.9) for OS and 1.1 (95% CI: 0.8-1.6;
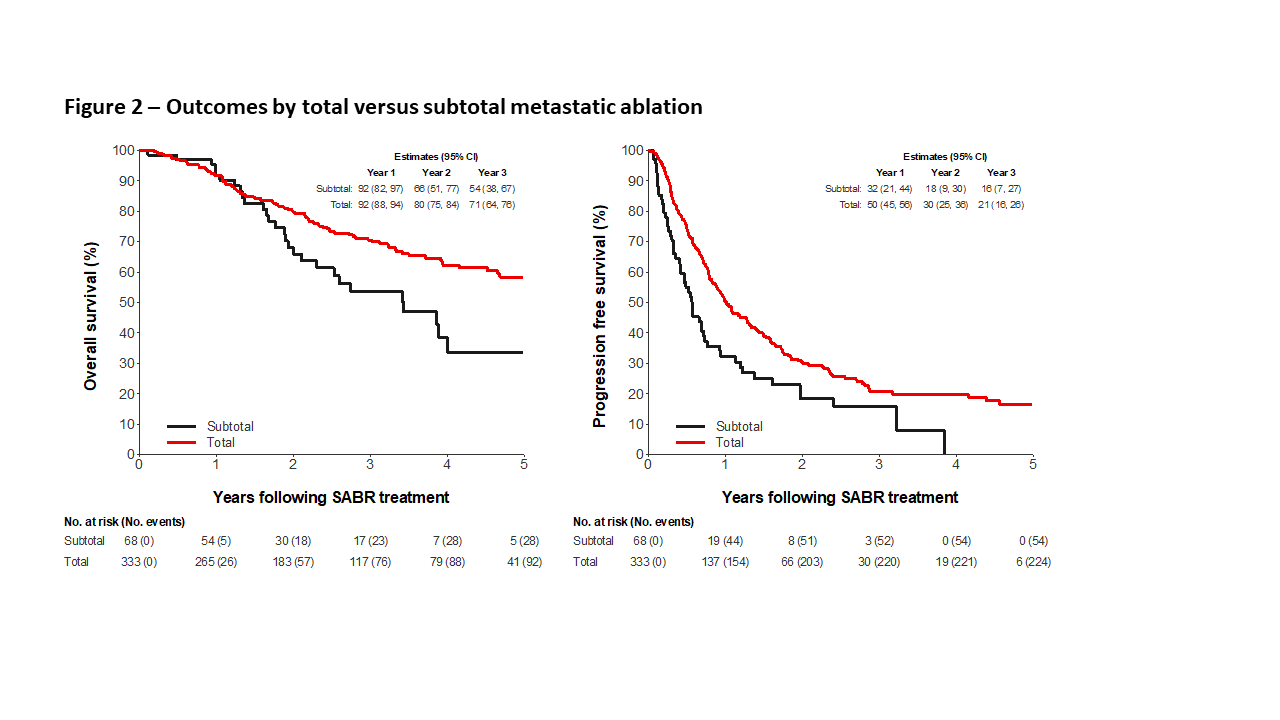
p=0.5) for PFS. Total metastatic ablation was prognostic for OS (logrank p=0.011)
and for PFS (logrank p=0.001), (Figure 2). The adjusted HR for OS was
0.8 (95% CI: 0.4-0.9; p=0.032) and for PFS was HR 0.6 (95% CI: 0.4-0.8; p=0.003).
Conclusion
Medical operability is not independently
prognostic in our cohort with oligometastatic disease. Total metastatic
ablation is associated with an improved OS and PFS compared with subtotal
metastatic ablation. This data suggests that treatment of all sites of metastases
should be optimised.