Simultaneous integrated boost in short-course radiotherapy; a novel approach for rectal cancer
MO-0224
Abstract
Simultaneous integrated boost in short-course radiotherapy; a novel approach for rectal cancer
Authors: Sandra Vieira1, Oriol Parés1, Joep Stroom1, Carlo Greco1
1Champalimaud Foundation, Radiotherapy, Lisboa, Portugal
Show Affiliations
Hide Affiliations
Purpose or Objective
In
the era of growing interest for Total Neoadjuvant Treatment (TNT) in rectal
cancer several studies show improved oncologic outcomes by intensifying
chemotherapy regimens before surgery. However not every patient is fit for such
a strategy of chemo-intensification. Another element of the treatment of rectal
cancer with potential to be intensified is radiotherapy. We report on a new
approach with dose intensification through a simultaneous integrated boost
(SIB) in short-course preoperative radiotherapy for rectal cancer patients (SCRT).
Material and Methods
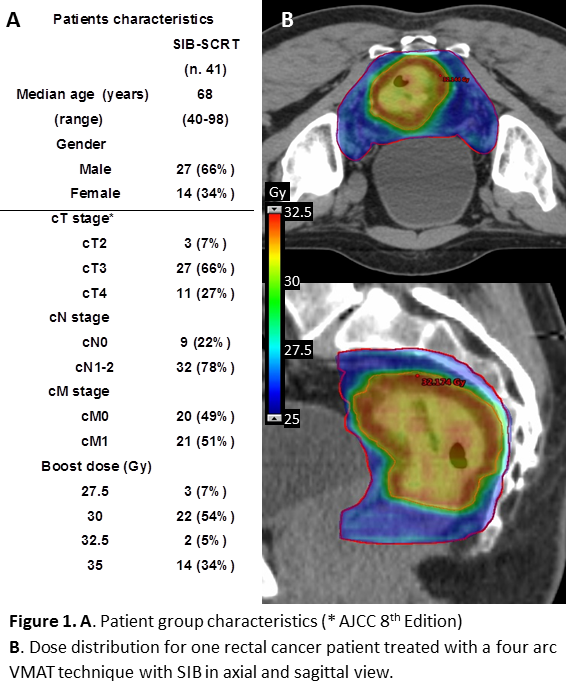
Between
February 2014 and June 2019, 41 patients with rectal adenocarcinoma (27 male,
14 female; median age 68 years), were treated with SIB-SCRT (fig1). Inclusion
criteria for SIB were advanced age, severe comorbidity precluding surgery, or
tumor high-risk features requiring prompt systemic therapy. The planning target
volume (PTVpelv) consisted of the mesorectum and lymphatic areas at
risk (CTVpelv+ 5mm) and received 25 Gy over 5 consecutive days, with
a SIB between 27.5-35 Gy on PTVboost (GTVboost+5mm) according
to the extent of the disease and proximity to OARs. A 4 arc 10FFF VMAT plan
(Eclipse™) was used (fig1). PTV coverage was defined as the volume receiving
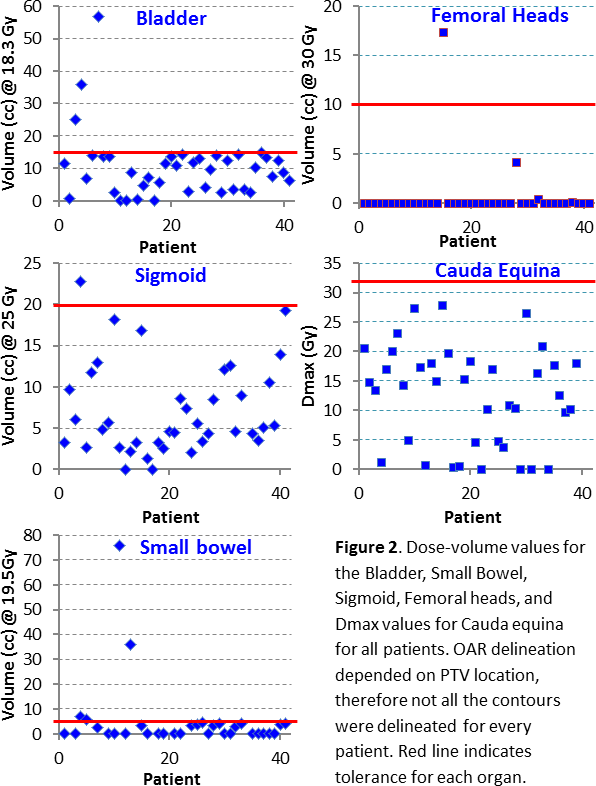
the prescribed dose. OAR dose constraints were derived from published hypofractionation
schemes: D5cc<19.5Gy, Dmax
35Gy for small bowel (SB); D15cc<18.3Gy for bladder (B) and
D20cc<25Gy for sigmoid (S), with Dmax 38Gy for both; D10cc<30Gy
for femoral heads (FH); and D5cc<30Gy, Dmax 32Gy for cauda
equina (CE). Pre-treament QA (ArcCheck®) was performed for all patients using
gamma (3%/3mm) passing rates >90%. Patients were set-up with CBCT imaging
for all fractions.
Results
At a median follow-up of 38 months
(mean 46±36), 23% of patients died of systemic disease progression. Treatment
was well-tolerated by all patients. Acute and late RTOG Gastrointestinal (GI)
score of grade 3 occurred in 14% and 0% of the cases (no grade 4), and
genitourinary (GU) grade 2 in 5% and 4% (no grade3), respectively. Mean CTV was
418±199cc and 57±46cc for the pelvis and the boost, respectively. Dose coverage
was 98±3% (PTVpelv) and 98±6% (PTVboost). SB and B sparing
was the main reason for reduced PTV coverage. Dose tolerances were met for all OAR
with a few exceptions for the B, S and SB (see fig 2), in order to preserve the
PTVpelv standard coverage level (25Gy). Dose to FH was exceeded for
one patient due to
encompassed bone metastasis within the treatment
field
. QA
results were fulfilled for all patients (99±1%), showing that tighter gamma passing
rate criteria can be applied.
Conclusion
Dose
intensification in short-course RT for rectal cancer is a new, feasible and
safe approach to be considered in selected rectal cancer patients. Whether SIB-SCRT
can achieve higher rates of clinical or pathological responses compared to the
standard long-course chemoradiotherapy needs to be evaluated prospectively in
randomized clinical trials.