Simulation-CT Skeletal Muscle Index as a Biomarker for CRT compliance and survival in rectal cancer
MO-0223
Abstract
Simulation-CT Skeletal Muscle Index as a Biomarker for CRT compliance and survival in rectal cancer
Authors: Sara Reina1, Giuditta Chiloiro1, Marco Cintoni2, Barbara Corvari1, Elisa Meldolesi1, Emanuele Rinninella3, Gabriele Pulcini4, Marta Palombaro4, Antonio Gasbarrini5, Maria Cristina Mele4, Vincenzo Valentini1, Maria Antonietta Gambacorta1
1Fondazione Policlinico Universitario A. Gemelli IRCCS, UOC Radioterapia Oncologica, Rome, Italy; 2Università di Tor Vergata, Scuola di specializzazione in Scienza dell’Alimentazione, Rome, Italy; 3Fondazione Policlinico Universitario A. Gemelli IRCCS, UOC Nutrizione Clinica, Rome, Italy; 4Fondazione Policlinico Universitario A. Gemelli IRCCS, UOSD Nutrizione Avanzata in Oncologia, Rome, Italy; 5Fondazione Policlinico Universitario A. Gemelli IRCCS, UOC di Medicina Interna e Gastroenterologia, Rome, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Preoperative chemoradiotherapy (nCRT) in combination with total mesorectal excision (TME) is the standard treatment for patients with locally advanced rectal cancer (LARC). Nutritional status proved to be an effective prognostic marker in gastrointestinal malignancies. The aim of this study was to investigate the prognostic impact of a low skeletal muscle mass (SMM) before nCRT in LARC patients in terms of compliance to treatment and survival outcomes.
Material and Methods
LARC patients treated with nCRT in our institution between 2010 and 2020 were retrospectively collected and analyzed. Before the start of nCRT, all patients performed a simulation Computed Tomography (CT)-Scan. All patients underwent long course RT with different concomitant CT schedule. Skeletal Muscle Area (SMA), defined as the total muscle area of bilaterally erector spinae, quadratus lumborum, psoas, internal and external obliques, transversus abdominis, and rectus abdominis, was obtained by a single slice at the level of the third lumbar (L3) vertebra on the simulation CT-Scan. Skeletal Muscle Index (SMI) was calculated normalizing SMA by height squared. Sarcopenic obesity was diagnosed when an overlap between obesity (BMI≥30) and a low SMI was found. nCRT compliance was considered in terms of RT interruption and GI toxicity≥3, according to Common Terminology Criteria for Adverse Events (CTCAE) v5.0. Multivariable Cox regression model was constructed, including all variables with p<0.05 at univariate analysis, to assess differences among overall survival (OS). Logistic univariate and multivariate regression analysis was used to identify factors independently associated with RT interruption.
Results
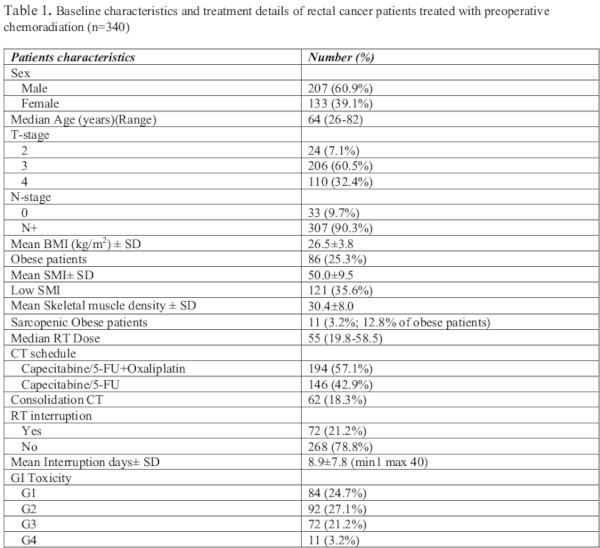
Overall 340 LARC patients (60.9% male, 39.1% female; median age 64) were enrolled for final analysis (Table1). Median RT dose on tumor was 55 Gy. 62 patients (18.3%) received consolidation chemotherapy during the surgical interval. Mean SMI was 50.0±9.5 and 121 patients (35.6%) were sarcopenic. The population included 86 (25.3%) obese patients, and 12.8% of those had low SMI (sarcopenic obese patients). 72 patients (21.2%) had temporary treatment interruption due to toxicity; mean interruption days was 8.9±7.8. The incidence of Grade≥ 3 lower gastrointestinal acute toxicity was 24.4%.
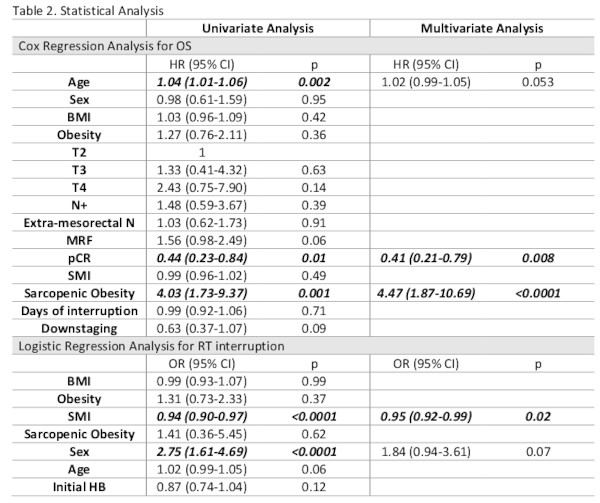
SMI resulted as an independent factor for nCRT interruption (OR: 0.95, 95% CI 0.92-0.99; p=0.02). At multivariate Cox regression analysis, pCR (HR:0.41, 95% CI 0.21-0.79; p=0.008) and sarcopenic obesity (HR:4.47, 95% CI 1.87-10.69; p<0.0001) resulted as independent factors for OS (Table2).
Conclusion
Low SMI appear to be a resourceful and economic biomarker for nCRT compliance, in terms of RT interruption; furthermore, in the setting of obese patients, a low SMI significantly affects OS. By the analysis of this feature, easily obtainable from the simulation CT, result the possibility to improve the patient's compliance and the survival of the obese patient, personalizing patient’s nutritional support before and during the treatment.