Hypofractionated versus conventional adjuvant radiotherapy for lymph node metastases of melanoma
Lodewijka HJ Holtkamp,
The Netherlands
MO-0152
Abstract
Hypofractionated versus conventional adjuvant radiotherapy for lymph node metastases of melanoma
Authors: Lodewijka HJ Holtkamp1,2, Serigne N Lo1,3, Martin Drummond1, John F Thompson1,3,4, Omgo E Nieweg1,3,4, Angela M Hong1,3
1The University of Sydney, Melanoma Institute Australia, Sydney, Australia; 2University Medical Center Groningen, Department of Surgical Oncology, Groningen, The Netherlands; 3The University of Sydney, Faculty of Medicine and Health, Sydney, Australia; 4Royal Prince Alfred Hospital, Department of Melanoma and Surgical Oncology, Sydney, Australia
Show Affiliations
Hide Affiliations
Purpose or Objective
Adjuvant post-operative radiotherapy (RT) has been shown to reduce the risk of recurrence in a lymph node field following therapeutic dissection for high-risk stage III melanoma. However, the optimal fractionation schedule is unknown and both hypofractionated and conventionally fractionated adjuvant RT have been used. The aim of this study was to compare the oncological outcomes of these two approaches in an era before effective systemic immunotherapy became available. The primary endpoint was node field recurrence (as a first recurrence). Secondary endpoints were recurrence-free survival (RFS) and overall survival (OS). Risk factors associated with node field recurrence as a first recurrence, RFS and OS were also assessed.
Material and Methods
This retrospective, single-institution study involved 335 patients with stage III melanoma who received adjuvant radiotherapy after therapeutic regional lymph node dissection for metastatic melanoma between 1990 and 2011. Information on tumour characteristics, radiotherapy and patient outcomes was retrieved from the Melanoma Institute Australia database and patients’ medical records.
Results
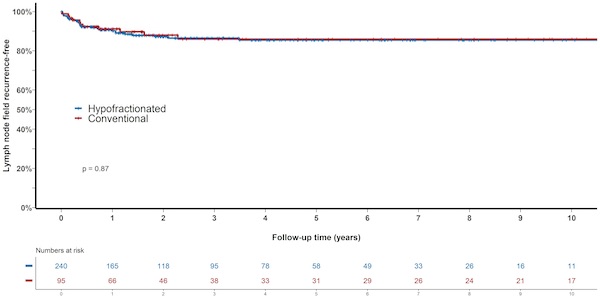
Hypofractionated RT (median dose 33 Gy in six fractions over three weeks) was given to 95 patients (28%) and conventionally fractionated RT (median dose 48 Gy in 20 fractions over four weeks) to 240 (72%). Five-year lymph node field control rates were 86.0% (95% CI 78.4-94.4%) in the hypofractionated group and 85.5% (95% CI 80.5-90.7%) in the conventional fractionation group (P=0.87), see figure. There were no significant differences in RFS (41.7% (95% CI 32.5-53.5) vs. 31.9% (95% CI 26.1-38.9), P=0.18) respectively, and OS (41.2% (95% CI 32.1-52.8) vs. 45.0% (95% CI 38.7-52.4) P=0.77). On multivariate analysis, extranodal spread was associated with decreased RFS (P=0.04). The number of resected lymph nodes containing metastatic melanoma was associated with decreased RFS (P=0.0006) and OS (P=0.01).
Conclusion
Lymph node field control rates, RFS and OS were similar after hypofractionated and conventionally fractionated adjuvant RT. The presence of extranodal spread and an increasing number of positive lymph nodes were predictive of an unfavourable outcome. Our results are particularly interesting in the light of recent studies that suggest an immunogenic effect when combining hypofractionated RT with checkpoint inhibition. Furthermore, a hypofractionated schedule would mean fewer treatment visits, which would be easier for patients and reduce demand on healthcare resources. Unfortunately, the retrospective nature of our study did not allow reliable assessment of acute and late toxicity. Overall, the results warrant further investigation of RT fractionation in patients with melanoma.