RTT Best Paper: Predicted reduction in ΔNTCP by model based selected proton therapy for oesophageal cancer patients
Petra Klinker,
The Netherlands
OC-0508
Abstract
Predicted reduction in ΔNTCP by model based selected proton therapy for oesophageal cancer patients
Authors: Petra Klinker1, Erik Korevaar1, Annamieke Koops1, Margriet Dieters1, Véronique Mul1, Anne Niezink1, Johannes Langendijk1, Christina Muijs1
1University Medical Centre Groningen, University of Groningen, Radiation Oncology, Groningen, The Netherlands
Show Affiliations
Hide Affiliations
Material and Methods
MBS requires
a plan comparison (PhRT vs PRT) which was performed in all EC patients. To select patients for PRT, the
following eligibility criteria had to be met: cT1-T3, cN0-N2, WHO performance score
<2, target motion <15 mm (established on 4DCT) and a ΔRisk >5% for 2-years
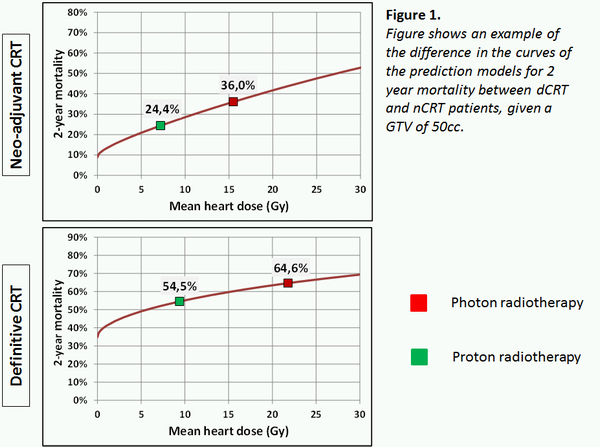
mortality. We used the following prediction models for 2-years mortality;
for
dCRT: -1.0421 + 0.059 * SQRT (GTV) + 0.263 * SQRT (MHD),
and for
nCRT: -3.0352 + 0.100 * SQRT (GTV) + 0.4457 * SQRT (MHD).
IMPT robustly
optimized plans were created using a 3 beam approach including 5 times
repainting to reduce the impact of intra-fractional motion during treatment. To
verify patient positioning, daily 2DKV imaging, online CBCT’s and weekly repeat
CT’s were performed.
Results
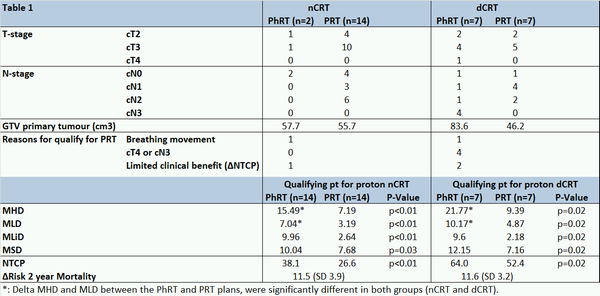
Since July 2021, 30 patients were treated with nCRT (n=16) or dCRT (n=14) for EC at our department. In total 21 patients (70%) qualified for PRT, including 88% of patients treated with nCRT and 50% of those treated with dCRT. Reasons for not qualifying were mostly N3-status in the dCRT group and breathing movement and limited clinical benefit in the nCRT group (Table 1). In patients who qualified, the mean heart (MHD), lung (MLD), liver (MLiD) and spleen dose (MSD) were significantly lower for PRT compared to PhRT. Although, the ΔMHD (12.4 vs 8.3 Gy) and ΔMLD (5.3 vs 3.8 Gy) between the PhRT and PRT plans were significantly larger in dCRT group compared to the nCRT group, the difference in the 2-year mortality risk was on average 12% in both groups, in favour of PRT. This might be explained by the difference in the steepness of and the position on the curves of the prediction models for dCRT or nCRT (Figure 1).
Conclusion
PRT reduces the dose in multiple organs-at risk,
including the MHD. Using the applied model, this is expected to result in reduced
mortality risk, both after nCRT and dCRT. Criteria, other than ΔRisk, seem to impact the
selection of EC patients for PRT more often in the dCRT group.