Physics Best Paper: Salivary gland dose response modelling using PSMA PET/CT
Vineet Mohan,
The Netherlands
OC-0506
Abstract
Salivary gland dose response modelling using PSMA PET/CT
Authors: Vineet Mohan1, Natascha Bruin2, Jeroen van de Kamer1, Jan-Jakob Sonke1, Wouter Vogel2
1Netherlands Cancer Institute, Radiation Oncology, Amsterdam, The Netherlands; 2Netherlands Cancer Institute, Radiation Oncology and Nuclear Medicine, Amsterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Xerostomia remains a
common side effect of radiotherapy (RT) for patients with head and neck
(H&N) cancer despite advancements in treatment planning and delivery.
Molecular PET imaging of the prostate specific membrane antigen (using 68Ga/18F-PSMA)
is highly specific to prostate cancer, but uptake in salivary glands reflects
the presence of generally abundantly PSMA-positive secretory cells. We aimed to
objectively quantify the dose-response of salivary glands using PSMA PET.
Material and Methods
30 H&N cancer patients
were included in a prospective study. They received RT with 70 Gy in 35
fractions over 7 weeks. PSMA PET/CT was acquired in treatment position at
baseline and at 6-months post-RT. The PET scans were deformably registered to
the planning CT and the associated dose distribution. Dose, pre-RT SUV and
post-RT SUV were extracted for every voxel inside each delineated parotid salivary
gland. The data was analysed using a generalised linear mixed effects model
using a log link.
Results
Fig. 1 shows the dose
distribution, and baseline and post-RT PSMA PET images of one patient. The
baseline SUV was observed to moderate the effect of dose on the post-RT SUV.
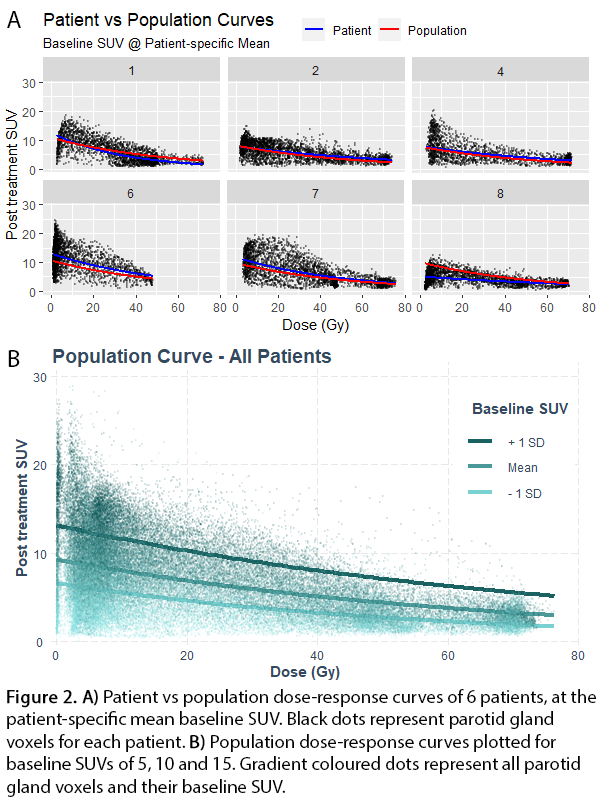
The population and patient-specific dose-response curves for the parotid glands,
can be seen in Fig. 2. The model fit the data well with an R2 of
0.79. The D50 of the population-curve is 34 Gy. The population curve
indicates that for a 1 Gy increase in dose, the post-treatment SUV decreases by
1.8%, for a baseline SUV of 10. 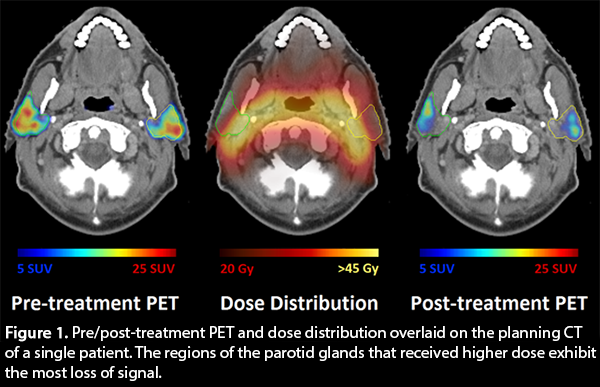
Conclusion
The PSMA PET response
in salivary glands after RT demonstrates a strong relationship between dose and
loss of secretory cells. Differences in patient sensitivity can also be
observed, which the model can account for. The population curve could
potentially be used in dose planning, using a planning objective to maximize the
predicted post-treatment SUV. This could be improved upon further by using a
pre-treatment PSMA scan to get patient-specific curves.