ESTRO-Elekta Brachytherapy Award: HDR brachytherapy boost improves metastatic free survival in high and very-high risk prostate cancer
Ignacio Visus,
Spain
OC-0611
Abstract
HDR brachytherapy boost improves metastatic free survival in high and very-high risk prostate cancer
Authors: Ignacio Visus1, Andrea Barco1, Jorge Obeso2, Marta Barrado1, Amaya Sola1, Elena Villafranca1, Naiara Fuentemilla3, Santiago Pellejero3, Paola Navarrete4, Enrique Martinez1
1Hospital Complex of Navarre, Radiation Oncology, Pamplona, Spain; 2Puerta del Hierro Mahadahona University Hospital, Radiation Oncology, Madrid, Spain; 3Hospital Complex of Navarre, Medical Physics, Pamplona, Spain; 4Valdecilla University Hospital, Radiation Oncology, Santander, Spain
Show Affiliations
Hide Affiliations
Purpose or Objective
To assess the impact of HDR brachytherapy boost (HDR-BT) against exclusive external beam radiotherapy (EBRT) in biochemical free survival (BFS) and metastatic free survival (MFS) in high-risk prostate cancer patients. We also analyse differences in the HDR-BT impact in MFS between high-risk patients and very-high-risk patients.
Material and Methods
We performed a retrospective analysis of patients diagnosed with high and very-high risk prostate cancer. One group received exclusive EBRT including pelvis with a prostate dose of 77,4-78 Gy while another group received 46-54 Gy followed by a HDR-BT in 2 fractions of 7.5Gy or single fraction of 15 Gy. External radiotherapy in both groups was delivered with IMRT in 82% of patients. Androgen deprivation therapy was administered during 2.5 years. Survival rates and multivariate analysis were performed using Kaplan Meier and Cox regression models with SPSS v25. Toxicity was analyzed with CTCAE version 5.0 criteria.
Results
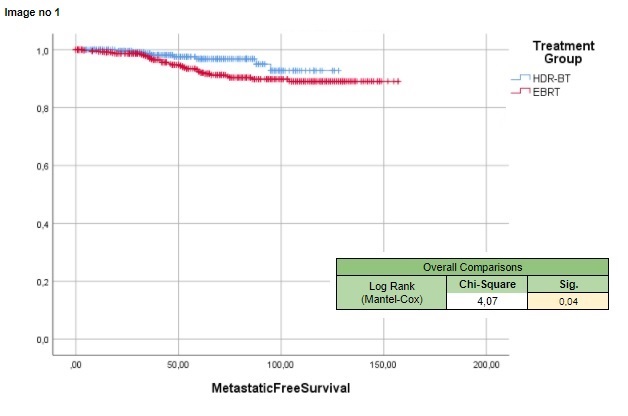
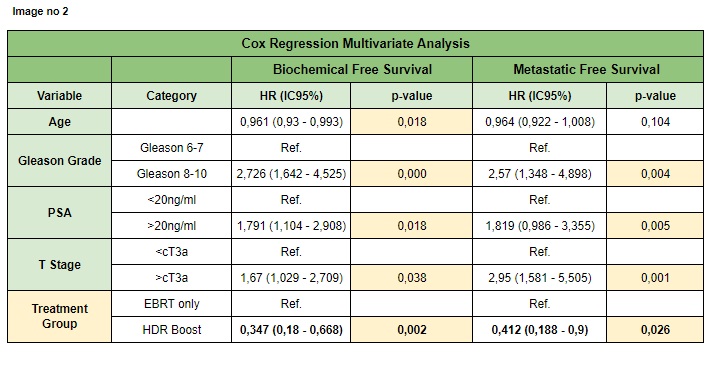
With a mean age of 69.8 years and a median follow up of 64 months, 801 patients treated in our department from 2008-2020 were included in the analysis, 481 patients (60.05%) in the EBRT group and 320 (39.95%) in the HDR-BT group. 5-year BFS was 96.4% in HDR-BT group and 89.2% in EBRT group (p 0.004). The 5-year MFS was 96.9% in HDR-BT group and 92.4% in EBRT group (p 0.04) (image1). We performed a multivariate analysis in order to adjust BFS and MFS in both treatment groups by age, histology, PSA level and T stage (image 2); we found for the HDR-BT group had a hazard ratio (HR) of 0.34 (CI95% 0.18-0.66; p 0.002) in BFS and a HR of 0.41 (CI95% 0.18-0.9; p 0,02) in MFS. The impact of HDR-BT in MFS was predominant in very-high-risk (log rank p 0.02) versus high-risk patients (log rank p 0.9), although the number of events was only 11 in high-risk and 31 in very-high-risk. Genitourinary toxicity: acute grade 2 or more was 1.73% and 3.22% in HDR-BT and EBRT group, whereas chronic toxicity was 3.34% and 3.11% respectively. Gastrointestinal toxicity: acute grade 2 or more was 3.22% and 2.07% in HDR-BT and EBRT group, whereas chronic toxicity was 1.27% and 3.45% respectively.
Conclusion
We found a benefit in metastatic survival in the HDR-BT boost group with a very acceptable grade of toxicity. HDT-BT should be considered standard of care in treatment for both high-risk and very-high risk prostate cancer patients. Although the HDR-BT impact in MFS was higher in very-high-risk patients, the differences were probably caused by the need for longer follow-up in high-risk patients.