Successful pregnancies after helical Tomotherapy craniospinal irradiation for adult medulloblastoma
OC-0589
Abstract
Successful pregnancies after helical Tomotherapy craniospinal irradiation for adult medulloblastoma
Authors: Elisa Coassin1, Loredana Barresi2, Cristina Cappelletto2, Alicia Tosoni3, Paola Chiovati2, Annalisa Drigo2, Alba Brandes3, Maurizio Mascarin1
1Centro di Riferimento Oncologico di Aviano (CRO) IRCCS, AYA Oncology and Pediatric Radiotherapy Unit - High Technology Department, Aviano, Italy; 2Centro di Riferimento Oncologico di Aviano (CRO) IRCCS, Medical Physics Division - High Technology Department, Aviano, Italy; 3IRCSS Istituto di Scienze Neurologiche di Bologna, Nervous System Medical Oncology Department, Bologna, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
A retrospective study was conducted to analyze fertility outcomes in adult medulloblastoma (MB) pts of childbearing age treated with helical Tomotherapy craniospinal irradiation (HT-CSI) at the Pediatric Radiotherapy Unit of the Centro di Riferimento Oncologico di Aviano (CRO) IRCCS in Aviano, Italy.
Material and Methods
From September 2006 to May 2021, 12 women of childbearing age (range 20-36 years, median 31) with MB underwent HT-CSI. The prescribed HT-CSI dose was 32.4 Gy (1.8 Gy/fr) for non-metastatic pts, and 36 Gy (1.8 Gy/fr) for metastatic pts, with a boost to the tumor bed and metastases. Administered chemotherapy (CT), performed fertility preservation techniques, menstrual activity, anti-Müllerian hormone (AMH) levels, and radiation doses to the ovaries were recorded. Successful pregnancies resulting in live births after HT-CSI were examined.
Results
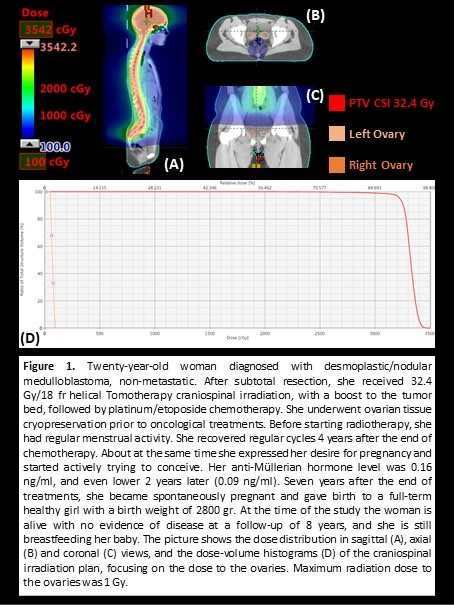
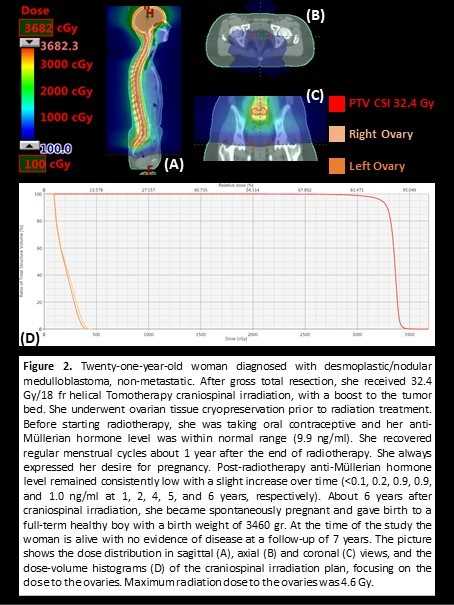
At the time of the study, all women were alive with a median fup of 4.4 years (range 0.8-10.4). A 31-year-old patient reported a 2-year history of secondary amenorrhea when diagnosed with MB and was excluded. Eight out of the remaining 11 pts were alive with NED with a median fup of 4.4 years (range 1.1-10.4) and were included in the analysis for fertility outcomes. Six non-metastatic pts received 32.4 Gy/18 fr HT-CSI; a subsequent whole spinal boost of 3.6 Gy/2 fr (to a total dose of 36 Gy/20 fr) was delivered to a platinum unsuitable patient; 2 metastatic pts received 36 Gy/20 fr HT-CSI, with one receiving a simultaneous integrated boost up to 45 Gy (2.25 Gy/fr) to the cauda equina region. Platinum/etoposide adjuvant CT was administered to 6 pts, together with gonadotropin-releasing hormone agonist (GnRH); 2 had no CT. Two pts underwent ovarian tissue cryopreservation prior to HT-CSI. Before starting RT, 5 pts had regular menstrual cycles, 2 were taking oral contraceptives, and 1 reported postpartum amenorrhea (4-month-old baby). Pre-RT AMH level was available for 3 pts, resulting <0.1 ng/ml for the postpartum amenorrheic woman (36 years old), and within normal range for the 2 women using oral contraceptives. Data on menstrual activity after finishing oncological treatments were available for 6 pts: 3 recovered regular cycles after 0.8-4 years, 2 still had irregular cycles at their last fup (at 10.1 and 2.5 years after therapy completion), and 1 was still amenorrhoic at the time of the study (5 months after suspension of adjuvant CT and GnRH). Median maximum radiation dose to the ovaries was 5.2 Gy (range 1.0-9.5 Gy). Only 2 women had actively tried to conceive after successful MB treatment. Both became spontaneously pregnant and gave birth to full-term healthy children. Patient and treatment characteristics and fertility outcomes of these 2 women are presented in Figure 1 and 2.
Conclusion
In this retrospective study of adult MB women of childbearing age, HT-CSI has not precluded 2 long-term survivors from becoming spontaneously pregnant and giving birth to healthy children.