Early adjuvant RT as a predictor of improved outcomes in patients with grade II and III meningiomas
Erica Maria Cuffini,
Italy
OC-0925
Abstract
Early adjuvant RT as a predictor of improved outcomes in patients with grade II and III meningiomas
Authors: Erica Maria Cuffini1, Chiara Casale1, Cristina Mantovani1, Alessio Gastino1, Bruna Lo Zito1, Ludovica Blasi1, Diego Bongiovanni1, Erika Orlandi1, Marzia Cerrato1, Angelisa Vella1, Silvia Leardi1, Valeria Chiofalo1, Chiara Cavallin1, Giuseppe Carlo Iorio1, Umberto Ricardi1, Mario Levis1
1University of Torino, Department of Oncology, Torino, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
Meningiomas are the most common primary intracranial
tumors. While WHO grade 1 meningiomas can be cured by surgical resection alone,
adjuvant radiotherapy (AdjRT) after surgery is recommended in WHO grade 3
(anaplastic). The role of AdjRT for atypical meningiomas (WHO grade 2) is still
unclear. This study aims to assess the impact of AdjRT on local control (LC), intracranial
progression free survival (PFS) and overall survival (OS) in patients with
diagnosis of atypical or anaplastic meningioma.
Material and Methods
We retrospectively collected patients with histologically
proven newly diagnosed or recurrent WHO grade 2 or 3 meningiomas, who underwent
gross total or subtotal resection followed by fractionated AdjRT between 2010
and 2020 at our institution. Response to treatment was evaluated through MRI,
according to RECIST criteria. LC, PFS and OS were estimated from the last day
of RT using the Kaplan-Meier method and stratified for possible prognostic
factors (i.e. RT timing, degree of resection, Ki-67, tumor grading, PTV).
Results
Our retrospective analysis included a total of
92 patients. Of these, 49 were males (53%) and 82 (89%) were diagnosed with an atypical
meningioma. In 68 (74%) patients AdjRT was administered upfront following a
de-novo diagnosis of meningioma while 24 (26%) patients received AdjRT after
re-intervention for disease recurrence following previous surgery. Median age
at diagnosis was 62 years. Gross total and subtotal resection was achieved in
58 (63%) and 34 (37%) of patients respectively, with a median Ki-67 of 15%. Median
prescribed RT dose was 54 Gy (min 42 Gy, max 60 Gy) administered in daily
fractions of 1.8-3 Gy, with a median overall treatment time (OTT) of 44 days.
Median PTV volume was 163 cm3. With a median follow-up of 35 months, 3-year LC, PFS and OS were 80%, 73% and 90%, respectively. LC was
negatively affected by subtotal resection (p=0.002), Ki-67>15% (p=0.013),
high tumor grading (p=0.020) and PTV larger than 165 cm3 (p=0.021).
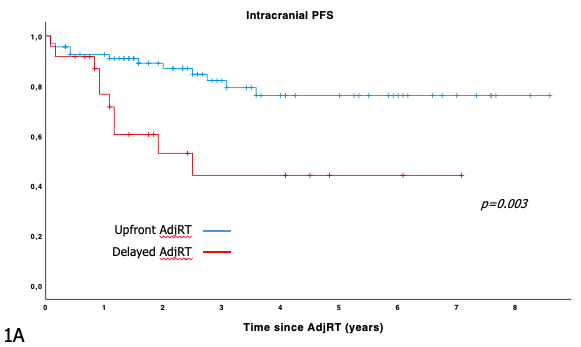
Patients receiving AdjRT after re-intervention had a lower PFS at 3 years
compared to those receiving AdjRT upfront after first surgery (82% vs 44%,
p=0.003, Figure 1A). Both subtotal
resection (p=0.005) and Ki-67>15% (p=0.005) negatively affected PFS.
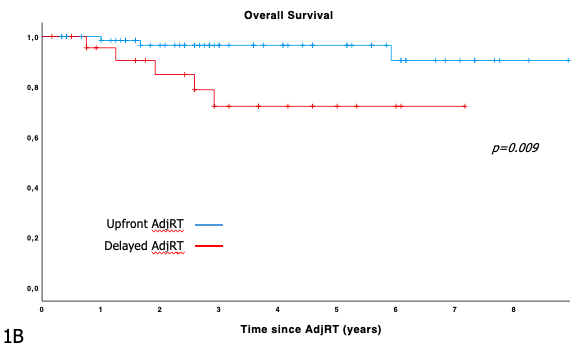
Finally, OS was negatively affected by Ki-67>15% (p=0.031) and by the timing
of AdjRT, with patients who underwent upfront AdjRT having a higher OS at 3
years compared to patients receiving delayed AdjRT after re-intervention (96%
vs 72% p=0.009, Figure1B).
Conclusion
Upfront adjuvant RT improves PFS and OS at 3
years in patients with WHO grade 2 and 3 meningiomas, whereas no statistically
significant difference was identified in terms of LC. Degree of resection,
Ki-67, tumor grading and PTV were also found to significantly affect patient
outcomes.