pseudoprogression after radiotherapy for IDH mutated low grade glioma in a multicenter photon cohort
Jaap Jaspers,
The Netherlands
OC-0924
Abstract
pseudoprogression after radiotherapy for IDH mutated low grade glioma in a multicenter photon cohort
Authors: Jaap Jaspers1, Walter Taal2, Jaap Zindler3, Annemarie Swaak1, Steven Habraken1, Mischa Hoogeman1, Remi Nout1, Martin van den Bent2, Alejandra Méndez Romero1
1Erasmus MC, Radiotherapy, Rotterdam, The Netherlands; 2Erasmus MC, Neuro - Oncology, Rotterdam, The Netherlands; 3Haaglanden MC, Radiotherapy, The Hague, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Several
pathophysiological processes other than disease progression may give rise to
contrast enhancing lesions on MRI imaging after radiotherapy for low grade
glioma. Whether these lesions are indicative of dose-dependent tissue damage is
subject of debate, especially after proton radiotherapy. However, data on
contrast enhancing lesions after photon radiotherapy is scarce and their interpretation
is often heterogeneous. We investigated new contrast enhancing lesions in a multicenter
cohort of historical patients with IDH mutated grade 2 diffuse glioma treated
with photon therapy, using a strict definition of pseudoprogression (psPD) and
disease progression (PD).
Material and Methods
Patients with
histologically confirmed IDH-mutated diffuse
grade 2 glioma treated with 50.4Gy between 1-1-2007 and 31-12-2018 were eligible
for this study. Patients were treated in two tertiary referral centers. All
MRI’s acquired between radiotherapy and PD were included and reviewed in the
study. PD was defined in accordance with the RANO criteria. PsPD was defined as
any new contrast-enhancing lesions between end of radiotherapy and PD, or any new
contrast-enhancing lesion that remained stable over a period of 12 months in
patients who did not exhibit PD. Lesions were described as transient if
resolution was observed during follow-up, and persistent if no resolution was
observed until PD or end of follow-up. Duration of psPD was defined as time
between first and last MRI that showed psPD. Kaplan Meier estimates were used for
overall survival from diagnosis (OS) and progression free survival (PFS) from end
of radiotherapy.
Results
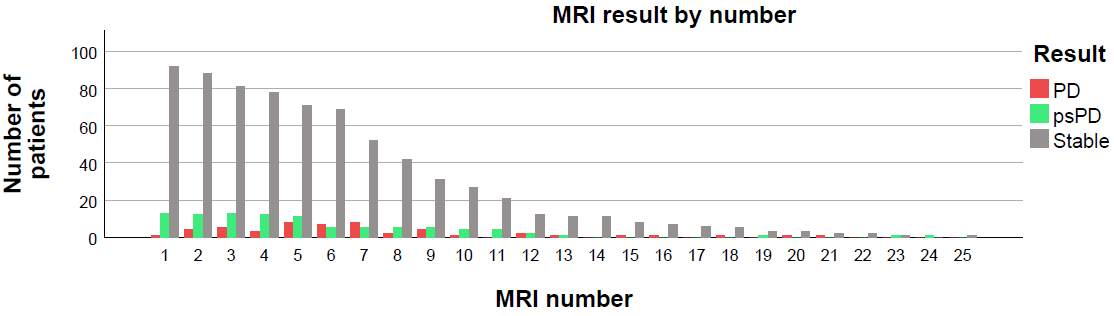
A total of 106 patients
were eligible and 931 MRI’s were analyzed. Median number of MRI’s per patient
was 8 (range 1 – 25). Median follow up duration from radiotherapy was 3.8 years
(range 0.3 – 12.7). A 1p19q codeletion was present in 46 patients (43.4%),
absent in 53 patients (50.0%), and unknown in 7 patients (6.6%). Adjuvant
chemotherapy was given to 52 patients (49.1%). At the time of analysis, median OS
was 10.7 years (95% CI 8.3 – 12.9) and median
PFS was 5.9 years (95% 4.9 – 7.0). PsPD was observed in 29 patients (27.4%) on at
least one MRI. Median onset of psPD was 8.4 months (range 0.9 -137.2). In
patients with psPD, 9 patients (31%) were found to have psPD on one MRI while 20
patients (69%) showed psPD over multiple MRIs (median 3, range 2-11). Median
duration of all psPD was 6.2 months (range 0 – 53.5). PsPD was transient in 22 of
29 patients (79.2%). Median duration of transient psPD was 4.5 months (range 0 -
53.5). 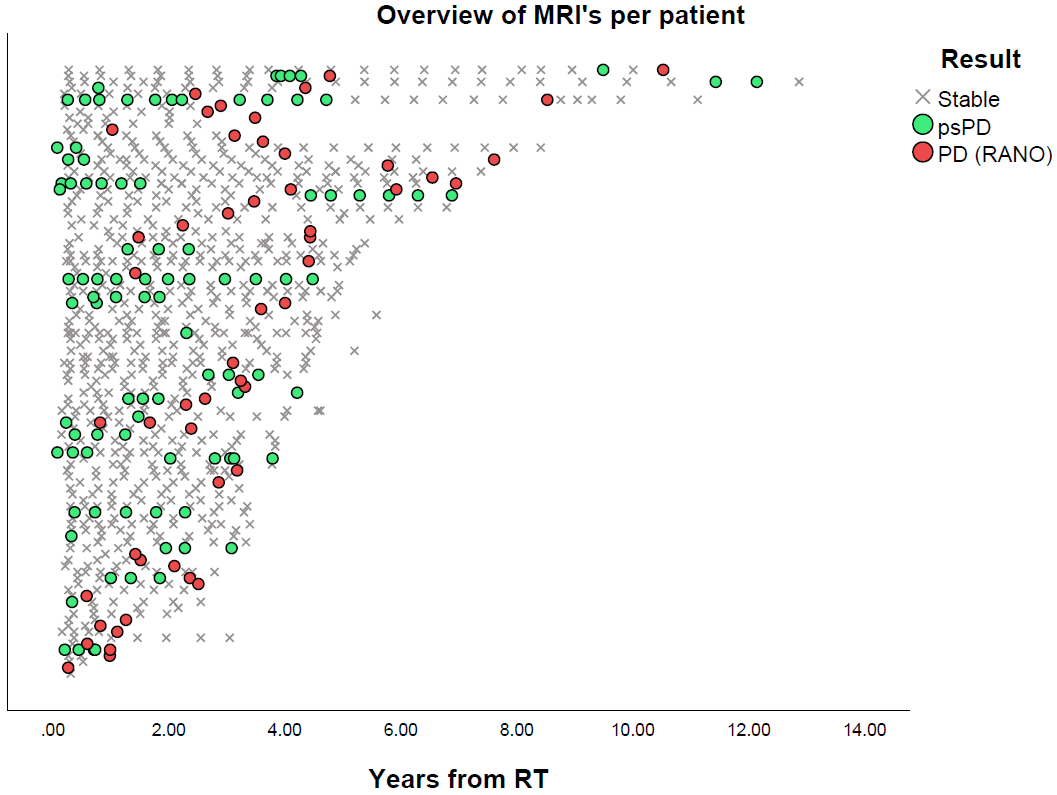
Conclusion
This study confirms
psPD occurs frequently in patients with IDH-mutated low grade after treatment
with photon radiotherapy. Although most PsPD occurs early in follow-up a
delayed presentation is also seen, possibly reflecting different pathophysiologic
processes. Awareness and identification of PsPD is warranted in patient care,
as well as when comparing outcomes among radiotherapeutic techniques.