Socioeconomic inequality in survival after oropharyngeal cancer – a nationwide study from DAHANCA
Maja Halgren Olsen,
Denmark
OC-0922
Abstract
Socioeconomic inequality in survival after oropharyngeal cancer – a nationwide study from DAHANCA
Authors: Maja Halgren Olsen1,2, Pernille Lassen1, Charlotte Rotbøl3, Kirsten Frederiksen4, Trille Kristina Kjær2, Jens Overgaard1, Susanne Oksbjerg Dalton2,5
1Aarhus University Hospital, Department of Experimental Clinical Oncology, Aarhus, Denmark; 2Danish Cancer Society Research Center, Survivorship and Inequality in Cancer, Copenhagen, Denmark; 3Aalborg University Hospital, Department of Oncology, Aalborg, Denmark; 4Danish Cancer Society Research Center, Statistics and Data Analysis, Copenhagen, Denmark; 5Zealand University Hospital, Department of Clinical Oncology & Palliative Care, Næstved, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
The socioeconomic inequality in survival after cancer
has increased during the past decades and is particularly pronounced for head
and neck squamous cell carcinoma (HNSCC). In the same period of time, the incidence of
HPV positive oropharyngeal
squamous cell carcinoma (OPSCC) has increased, while the prevalence of smoking
has decreased. This study
investigates socioeconomic differences
in survival after HPV positive and HPV negative OPSCC, respectively, and the
extent to which the socioeconomic gap in survival can be explained by
differences in smoking status, comorbidity and stage at diagnosis.
Material and Methods
Clinical information on all Danish patients registered with OPSCC between
2008 and 2019 in the population-based Danish Head and Neck Cancer Group
(DAHANCA) database were linked to nationwide, administrative registries, to obtain information
on individual level socioeconomic position, comorbidity and vital status. The effect of socioeconomic
position on five-year overall survival were estimated in Cox models adjusted
for age, sex and calendar year. The mediated proportion of smoking status,
comorbidity and stage at diagnosis were estimated based on the
counterfactual approach.
Results
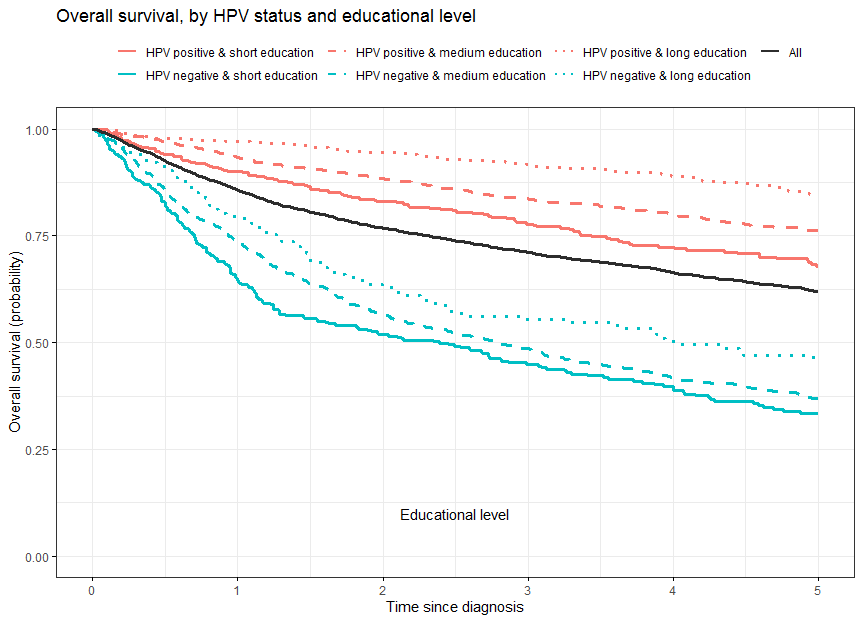
The five-year overall survival decreased gradually by
decreasing socioeconomic position, both among HPV positive and HPV negative
patients (Figure 1). The difference in five-year standardized survival
estimates between patients with low and high socioeconomic position was
approximately the same for HPV positive (-17.4 [95% CI: -22.0; -11.9]) and HPV
negative (-15.3 [95% CI: -23.7; -6.9]) patients. However, the estimated
mediated proportion of smoking varied, mediating 26.0% [95% CI: 16.8; 38.2] of
the observed inequality in survival among HPV positive patients and 6.5% [95%
CI: 1.4; 17.6] among HPV negative patients. Comorbidity mediated 14.1% [95% CI:
8.1; 22.8] and 12.7% [95% CI: 3.7; 30.8], respectively, whereas the mediated
proportion of stage at diagnosis was insignificant for both HPV positive (0.3%
[95% CI: -1.2; 2.1]) and HPV negative (8.4% [95% CI: -5.2; 26.8]) patients.
Combined, socioeconomic differences in smoking status, comorbidity status and
stage at diagnosis mediated 35.0% [95% CI: 25.0;50.1] among HPV positive
patients and 27.6% [95% CI: 11.4;61.8] among HPV negative patients.
Figure 1 Crude overall survival probability according
to HPV status and highest attained educational level, among Danish oropharyngeal squamous cell carcinoma patients registered
in DAHANCA, 2008-2019.
Conclusion
The socioeconomic gap in OPSCC survival is significant and
similar among patients diagnosed with HPV positive and HPV negative OPSCC. Most
of the effect of socioeconomic position on survival after OPSCC seems to work
via other pathways than those related to smoking status, comorbidity status and
stage at diagnosis. Differences in smoking behavior in particular may, however,
explain a considerable part of the socioeconomic inequality in survival after
HPV positive OPSCC.