National costs & resource requirements of radiotherapy: costing estimate from the ESTRO-HERO project
Katie Spencer,
United Kingdom
OC-0919
Abstract
National costs & resource requirements of radiotherapy: costing estimate from the ESTRO-HERO project
Authors: Tom Roques1, Katie Spencer2, Noemie Defourny3, Patricia Diez4, Angela Francis5, Sarah Griffin6, Keith Langmack7, Norman Kirkby3, Tom Mee3, Catherine Roe8
1Royal College of Radiologists, Faculty of Clinical Oncology , London, United Kingdom; 2University of Leeds, Academic Unit of Health Economics, Leeds, United Kingdom; 3University of Manchester, School of Medical Sciences, Manchester, United Kingdom; 4National Radiotherapy Trials Quality Assurance Group, Mount Vernon Cancer Centre, Radiotherapy Physics, Northwood, United Kingdom; 5Guy's and St Thomas' NHS Foundation Trust, Radiotherapy, London, United Kingdom; 6Royal College of Radiologists, Faculty of Clinical Oncology, London, United Kingdom; 7Nottingham University Hospitals NHS Trust, Radiotherapy Physics, Nottingham, United Kingdom; 8NHS Digital, National Radiotherapy Dataset, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
To estimate the cost of external beam radiotherapy in England in 2017 using a time-driven activity-based costing method
Material and Methods
The ESTRO-HERO model was populated with data from England in 2017 by a multi-professional team from seven radiotherapy centres. The number of courses and fractions for each indication was extracted from the national radiotherapy dataset with accurate data from each of the 52 English centres. Personnel numbers were taken from national censuses for each profession. Optional steps (motion management, immobilisation etc) were aggregated from at least 5 radiotherapy centres of different sizes. The time taken for tasks as part of RT preparation, planning and treatment were estimated based on data from two centres revised in consensus with the team. Personnel, equipment and infrastructure costs were obtained from publicly available and internal National Health Service (NHS) sources where available or consensus of the team. Sensitivity analyses were carried out where estimates were particularly uncertain.
Results
The total cost for radiotherapy in England was €680m. Of this, 67.3% was core costs of radiotherapy based on time and activity data, the largest component of which was the cost of treatment machines. 21.9% was supporting costs necessary to run a department (eg QA systems) and 10.8% was activities performed by radiotherapy personnel within the multidisciplinary oncology team such as attending tumour board meetings. The average cost of a course of radiotherapy was €4092. HERO estimates for costs of different treatments were usually slightly higher than reimbursement departments currently receive via the NHS tariff system.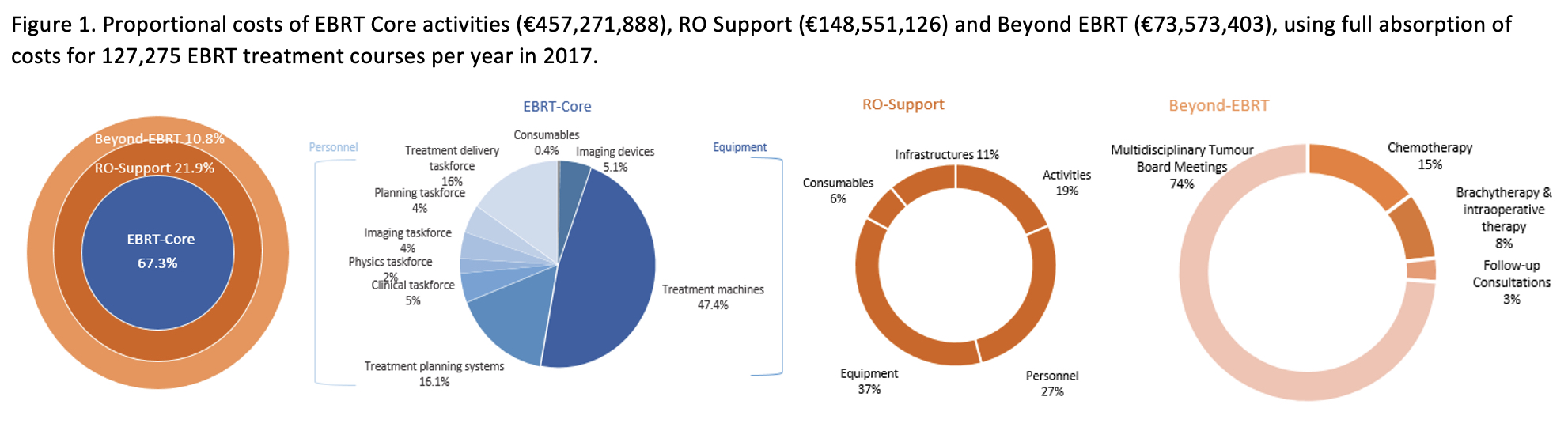
Conclusion
Radiotherapy is a relatively small part of the total NHS cancer budget (estimated to be approx. €7.1bn). These cost estimates can now be used to support analyses of cost-effectiveness, help refine the NHS reimbursement process and inform government investment decisions regarding both equipment and personnel. That treatment machine costs are such a high proportion of the total would support a national linac replacement programme with central procurement whilst the significant impact of bunker costs necessitates careful consideration of the mechanism of future capital funding.
By combining these data with estimates of future cancer incidence, this model will also help future workforce modelling recognising the resource implications of changing demand, new fractionation patterns and evolving techniques.