Mandibular osteoradionecrosis after postoperative radiotherapy for oral cavity cancer
Michelle Möring,
The Netherlands
MO-0481
Abstract
Mandibular osteoradionecrosis after postoperative radiotherapy for oral cavity cancer
Authors: Michelle Möring1,2,3, Hetty Mast2, Eppo Wolvius2, Gerda Verduijn1, Steven Petit1, Nienke Sijtsema1,4, Brend Jonker2, Remi Nout1, Wilma Heemsbergen1
1Erasmus MC Cancer Institute, Erasmus University Medical Center, Radiotherapy, Rotterdam, The Netherlands; 2Erasmus University Medical Center, Oral and Maxillofacial Surgery, Rotterdam, The Netherlands; 3Da Vinci Clinic, Hyperbaric Oxygen Therapy, Rotterdam, The Netherlands; 4Erasmus University Medical Center, Radiology and Nuclear Medicine, Rotterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Osteoradionecrosis (ORN) of the mandible is a severe
late complication of external beam radiotherapy (EBRT) for oral cavity cancer (OCC) that is
difficult to manage and can have a significant impact on quality of life. Several
risk factors for the development of ORN for head and neck cancers have been
identified, however, knowledge of risk factors for ORN after postoperative EBRT
(PORT) for OCC is limited. The goal of this study was to describe the incidence
and determine risk factors of mandibular ORN in patients treated with PORT for OCC.
Material and Methods
All OCC patients (N=227) treated with PORT at
the Erasmus Medical Center between 2010 and 2018, with a minimum of one year
disease free follow-up, were included in a retrospective cohort. The median age
was 66 (range 24-91), 58.6% was male, and 48.9% of the primary surgeries involved a
marginal or segmental mandible resection. Frequently prescribed dose schedules
were 33x2Gy (49.3%) and 30x2Gy (27.8%). Follow-up was censored at the first of
the following events: end of follow-up (standard follow-up 5 years), death, disease
recurrence or additional head and neck RT. Dose-volume data were extracted from
treatment plans. Cumulative incidence rates of mandibular ORN were computed
using the Kaplan Meier method. Risk
factors for
the development of mandibular ORN
were evaluated with Cox
regression models (uni- and multivariable).
Results
We observed
41 cases of ORN of the mandible (crude incidence 18.1%, 39 within 5 years),
with 13 mandibular fractures (31.7%) and 15 patients with orocutaneous fistulas
(36.6%). 92.7% of patients were symptomatic or required treatment (CTCAE grade ≥2). The Notani score (based on panoramic
radiograph), was available for 35 patients (87.8%), with N=18 Grade 3, N=10
Grade 2 and N=7 Grade 1. The estimated cumulative incidence was 8.4% (SE 1.8) at 1 year, 15.9% (SE 2.5) at 3
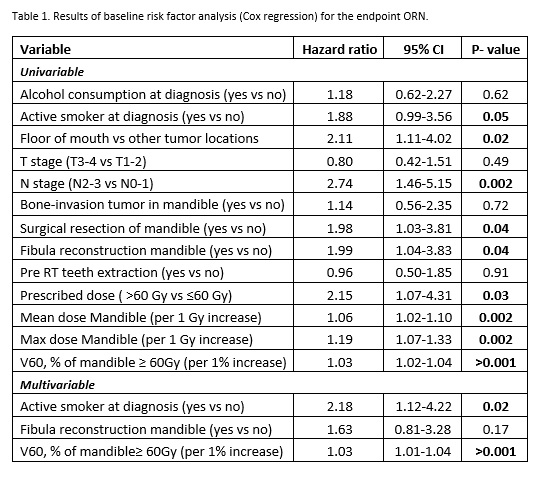
years, and 19.8% (SE 3.0) at 5 years (Figure 1). Univariable analysis (Table 1)
showed that being an active smoker at diagnosis, N-stage, any mandible
resection as primary surgery, fibula reconstruction of the mandible and tumor location at the
floor of mouth, were significantly associated with increased ORN risk. Looking
at dosimetric factors, we found that the Dmean of the mandible was higher in
patients with ORN (mean 41.1 Gy) than in patients without ORN (35.6 Gy). This
was similar for the DMax (69.4 Gy vs 65.7 Gy)
and V60 (37.9% vs 22.9%). Multivariable
analysis (HR, 95% CI) showed that smoking at diagnosis (2.17,
1.12-4.22)
and V60 (1.03, 1.01-1.04) remained
significant risk factors.
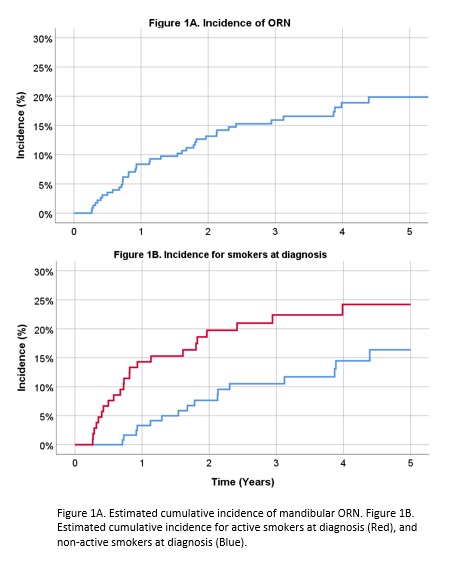
Conclusion
Patients
treated with PORT for OCC are at
high risk for ORN, with a 5-year cumulative incidence of 19.8%. Smoking
at diagnosis significantly increases the risk, with a 2.18
times higher chance of developing ORN. We also found a strong relation with mandibular
RT dose. We found that even small changes in treatment planning can decrease
the risk of ORN, as a 1% increase of V60 leads to a patient being 3% more
likely to develop ORN.