Simple strategy to select head and neck cancer patients for adaptive radiotherapy in the first week
Charlotte Brouwer,
The Netherlands
MO-0475
Abstract
Simple strategy to select head and neck cancer patients for adaptive radiotherapy in the first week
Authors: Yong Gan1, Johannes A. Langendijk1, Arjen van der Schaaf1, Lisa van den Bosch1, Edwin Oldehinkel1, Zhixiong Lin2, Stefan Both1, Charlotte L. Brouwer1
1University of Groningen, University Medical Center Groningen, Department of Radiation Oncology, Groningen, The Netherlands; 2Shantou University, Cancer Hospital of Shantou University Medical College, Department of Radiotherapy, Shantou, China
Show Affiliations
Hide Affiliations
Purpose or Objective
Adaptive radiotherapy (ART) enables correction of dose
deviation in organs at risk (OARs) caused by anatomic changes during head and
neck RT. The intensive workload for ART requires early identification of head
and neck cancer (HNC) patients that benefit most during radiotherapy, not only
to save workload/resource, but also to improve therapeutic ratio. The purpose
of this study was to present a simple strategy to select candidate of ART in
the first week of radiotherapy.
Material and Methods
This retrospective analysis was based on 123 HNC
patients who underwent photon radiotherapy and had at least 5 weekly in-treatment
re-scan CTs (rCTs) available. In total, 15 OARs were segmented on each rCT using
a semi auto-segmentation method (Gan et al., 2021). Then, the original treatment plan (VMAT or
IMRT) was re-calculated on each rCT with full scale of prescription dose to
obtain the actual weekly mean dose (Dmean) of OARs. The actual given
Dmean was defined as the average of all actual
weekly Dmean. We then applied the comprehensive NTCP-profile for HNC patients (van den Bosch et al., 2021)to translate the planning
Dmean and actual given Dmean into nominal and actual NTCP
values, respectively. The ΔNTCP were
obtained by subtracting nominal NTCP with actual NTCP values. The ΔDmean
between the first
weekly actual Dmean and
planning Dmean was calculated
and designated as ΔDmean_week1. For each ΔNTCP, the maximum ΔDmean_week1
of OARs which were
involved in the NTCP model was designated as maxΔDmean_week1.
The maxΔDmean_week1
was then used to develop different
logistic regression models to identify suitable candidates of ART who presented
large ΔNTCP with different criterion ΔNTCP from 0 to 10 of percentage point. For
different ΔNTCP criterion, the cutoff maxΔDmean_week1 was calculated (R program package of
pROC) to obtain the maximum summation of sensitivity and specificity, patients
presenting ΔDmean_week1 of any OAR ≥ the cutoff maxΔDmean_week1 were designated as classified candidate of ART, patients presenting any ΔNTCP
≥ criterion of ΔNTCP were classified as true candidate of ART. Major ΔNTCP was
defined as ≥5% and considered clinically relevant.
Results
In total, 7832 complete cases of NTCP values for different
kinds of toxicity in the 6th, 12th, 18th and
24th month after the end of radiotherapy together with the corresponding
maxΔDmean_week1 were obtained. The Spearman’s rank correlation
coefficient between maxΔDmean_week1 and
ΔNTCP was 0.42 ( p-value
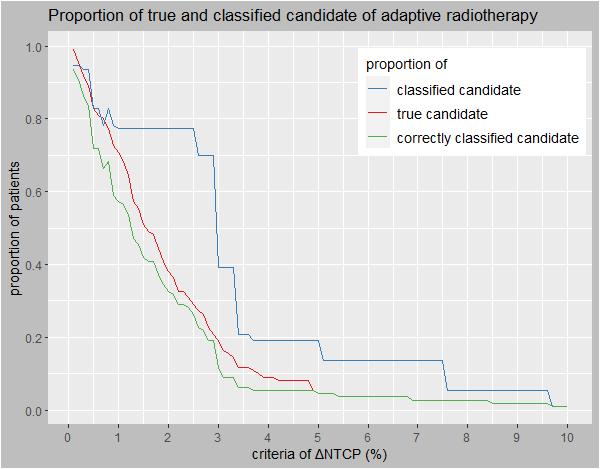
<0.001)(Fig.1). For major ΔNTCP, the cutoff maxΔDmean_week1 was 5.14Gy, the proportion of true candidate
of ART was 4.5%, the proportion of classified candidate of ART was 19.1% which included
all the true candidate of ART. (Fig.2).
Fig.1
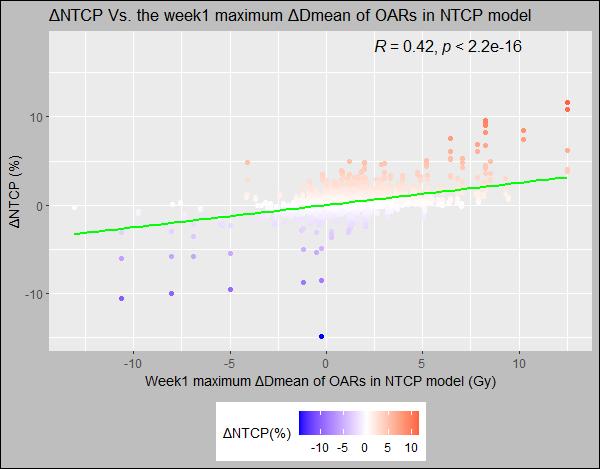
Fig.2
Conclusion
Using 5.14 Gy
as a cutoff value for ΔDmean of OARs in the first week enables
classifying all true candidates of ART who present ΔNTCP ≥ 5%, meanwhile correctly spares 80.9% of
patients from labor-intensive procedure of ART.