IGRT practice in the Netherlands: Does the current RTT curriculum need to be adapted?
Kim van Engen,
The Netherlands
OC-0461
Abstract
IGRT practice in the Netherlands: Does the current RTT curriculum need to be adapted?
Authors: Kim van Engen1,2, Martijn Kamphuis2, Mirjam Soumokil-de Bree2, Laila van Zadelhoff2
1Netherlands Cancer Institute, Radiation Oncology, Amsterdam, The Netherlands; 2Inholland University of Applied Sciences, Faculty of Health, Sports and Social work, Haarlem, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Image Guided (Adaptive) Radiation Therapy (IG(A)RT) is
constantly evolving. For educational institutes it is a continuous
process to adapt their curriculum to the actual clinical practice. It is
unclear whether the current IGRT curriculum is in line with the actual clinical
practice in RT departments in the Netherlands. The aim of this study is to
evaluate whether the curriculum suits the current and prospective professional
practice in IG(A)RT in the Netherlands.
Material and Methods
A survey was performed to evaluate current clinical
practice with regard to IG(A)RT. This was sent to all 21 main locations of RT
departments in the Netherlands. Several target areas were included in the
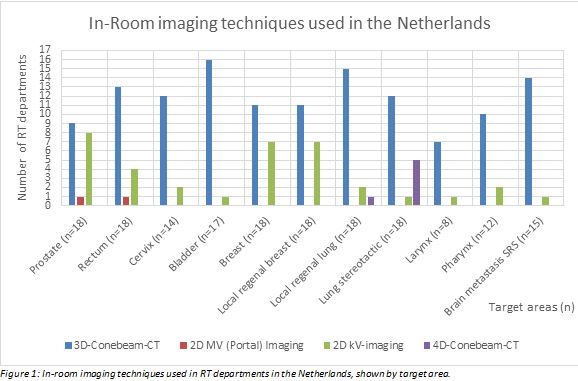
survey (Figure 1). Questions covered the use of following IGRT techniques:
• In-room imaging; 2D kV /2D MV (Portal) Imaging or
3D /4D Cone Beam CT (CBCT).
• Image guidance protocols; online
(translation/rotation(6D)/Library Of Plans (LOP)/adaptive), offline ((e)NAL/SAL).
• Match algorithms; Bone/Grey
value/Seeds/Mask/Manual.
• Determining match structures regarding target area.
• Protocol for anatomical/pathological changes.
Departments were asked about future developments
regarding new techniques and specifically if they intended to use Varian Ethos
or Magnetic Resonance Image guided Radiation Therapy
(MRIgRT). Target areas (in the progress
of) using these techniques were registered.
All survey results were anonymized and compared with
the current curriculum. Based on this, areas in need of improvement were
identified.
Results
A total of 18 (86%) respondents completed the survey (one
survey was incomplete). The most commonly used imaging technique was 3D CBCT,
while 2D MV (Portal) Imaging was barely used (Figure 1). All respondents used
online setup protocols, none used a fully offline setup protocol, and 28% (n=5)
used a combined online/offline protocol. Regarding adaptive strategies, LOP was
used or intended to be used for the bladder (55%, n=10), cervix (33%, n=6) and
rectum (11%, n=2). About 39% (n=7) of departments intend to use MRIgRT and 11%
(n=2) the Varian Ethos in the future. Every department had a protocol in place
for observed anatomical changes, of which 83% (n=15) used the traffic light
protocol. Except for MRIgRT,
all techniques clinically being used were present in the curriculum. However,
the traffic light protocol and LOP were only present to a limited extent.
Conclusion
The
IGRT curriculum is broadly in line with the current professional practice in
the Netherlands. However, some adjustments are advisable. 2D MV (Portal)
Imaging and offline setup protocols can become a smaller part of the IGRT
curriculum as these techniques are no longer frequently used. The use of
protocols dealing with anatomical changes, as well as the use of online
adaptive strategies (LOP/MRIgRT), should be included and more prominent in a future curriculum.