Fully automated adaptive multi-criteria planning for EMBRACE II cervical cancer brachytherapy
Rik Bijman,
The Netherlands
OC-0446
Abstract
Fully automated adaptive multi-criteria planning for EMBRACE II cervical cancer brachytherapy
Authors: Rik Bijman1, Linda Rossi1, Sebastiaan Breedveld1, Inger-Karine Kolkman-Deurloo1, Jan-Willem Mens1, Miranda Christianen1, Huda Abusaris1, Raymond de Boer1, Renee Rijnsdorp1, Michèle Huge1, Ben Heijmen1, Remi Nout1
1Erasmus Medical Center, Radiotherapy, Rotterdam, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
As
for external beam radiotherapy (EBRT), also for brachytherapy (BT) treatment
planning is a time-consuming task. Currently available commercial BT treatment
planning systems (TPS) require interactive trial-and-error dwell time optimization
to obtain an acceptable dose distribution, dependent on planner experience and allotted
time. We built a fully automated treatment planning workflow for adaptive
fractionated HDR BT for locally advanced cervical cancer after EBRT, in line
with EMBRACE II protocol planning aims and objectives. The system was validated
by comparing automated plans with manually generated clinical plans.
Material and Methods
Our
in-house TPS for automated multi-criterial plan generation for EBRT was
extended for HDR-BT. A process was developed to automatically establish daily
adaptive BT planning, based on delivered EBRT dose and BT doses of previous
fractions, following the EMBRACE II protocol and results in clinically
deliverable treatment plans. For 15 previously treated cervical cancer
patients, the clinical scans with contours and dwell positions of all 3 or 4 BT
applications were used and BT dose distributions were automatically generated,
with a high risk CTV (CTVHR) coverage equal to that in the clinical plan. Apart
from requirements for targets and OARs, there were also non-dosimetric
objective functions to prevent too high dwell time gradients and unbalanced
intracavitary, ovoid and interstitial needle usage. Fully automated adaptive BT treatment
planning was compared with clinical planning using EQD2Gy for the complete
treatment (EBRT+BT). Moreover, the sum of all dwell times (Efficiency), and the
ratio of dwell times outside CTVHR/sum of all dwell times (Outside/Total ratio)
were evaluated. Wilcoxon signed ranked test was used for statistical
evaluation.
Results
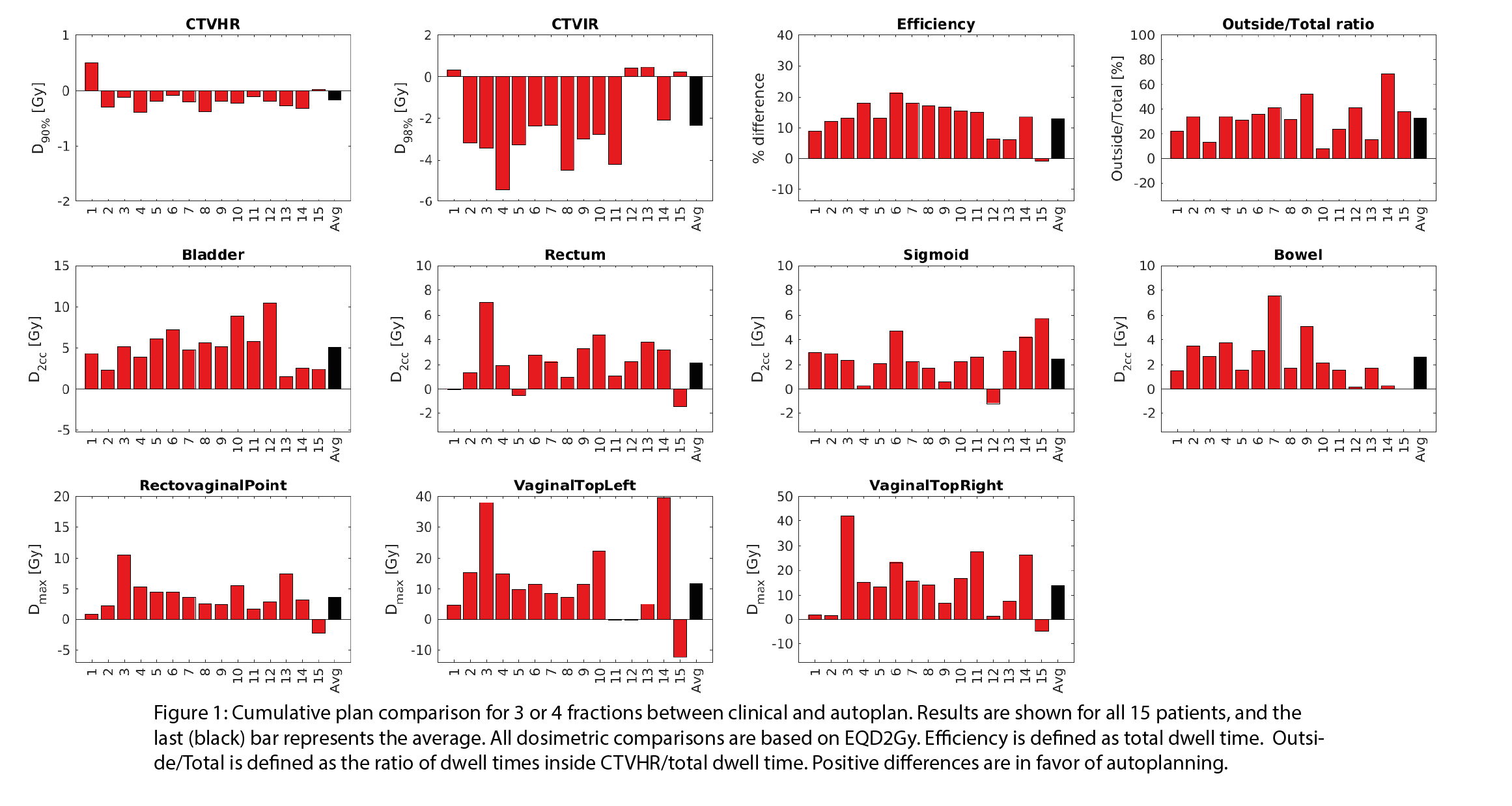
Autoplanning
resulted in lower OAR EQD2Gy compared to clinical planning for similar CTVHR coverage
(Figure 1). Intermediate risk CTV (CTVIR) coverage was lower with automated
plans compared to clinical plans, but always within protocol constraints. D2cc
for bladder, rectum, sigmoid and bowel were in favour of autoplanning with
average gains of 5.1 Gy [1.5 - 10.5 Gy, p<0.001] , 2.1 Gy [-1.5 - 7.0 Gy,
p=0.002] , 2.4 Gy [-1.2 - 5.8 Gy, p<0.001] and 2.6 Gy [0.2 - 7.6 Gy,
p<0.001], respectively. Moreover, large gains were also observed for the
rectovaginal point (3.7 Gy [-2.3 - 10.5 Gy, p<0.001]) and Dmax in
the vaginal tops left (11.7 Gy [-12.2 - 38.2 Gy, p=0.005]) and right (13.9 Gy [-4.7
- 42.2 Gy, p<0.001]). Autoplanning reduced the Efficiency on average by 13% with an Outside/Total ratio 33% lower compared to the clinical plans.
Optimization times for autoplanning were in the order of 3-6 minutes per plan.
Conclusion
Fully
automated adaptive multi-criteria planning for cervical cancer brachytherapy, according
to EMBRACE II protocol aims, resulted in improved total dose delivery (EBRT
+BT) compared to clinical manual planning. Plan generation took 3-6 minutes
with virtually zero workload.