Proton arc therapy with optimized settings reduces toxicity for head and neck cancer patients
Bas A. de Jong,
The Netherlands
OC-0453
Abstract
Proton arc therapy with optimized settings reduces toxicity for head and neck cancer patients
Authors: Bas A. de Jong1, Cecilia Battinelli2, Erik Engwall2, Guillaume Janssens3, Johannes A. Langendijk1, Erik W. Korevaar1, Stefan Both1
1University Medical Center Groningen, Department of Radiation Oncology, Groningen, The Netherlands; 2RaySearch Laboratories AB, Research and Development, Stockholm, Sweden; 3Ion Beam Applications SA, Research and Development, Louvain-la-Neuve, Belgium
Show Affiliations
Hide Affiliations
Purpose or Objective
Proton arc therapy has dosimetrical gains over conventional intensity
modulated proton therapy (IMPT) for diverse indications. A relationship exists between
normal tissue complication probability (NTCP), and the number of energy layers (ELs)
-and beams in a proton arc plan. This work aims to investigate the number of ELs
and beams required for optimal plan quality and impact on NTCP for
oropharyngeal cancer patients selected for IMPT.
Material and Methods
The RaySearch
energy layer reduction algorithm iteratively selects ELs from beams
equidistantly spaced over a 360 degree arc. The number of ELs and beams were
varied, to determine their relationship with NTCP and the estimated delivery
time for three patients. The delivery time was estimated for a “step and shoot”
type delivery, in which the gantry remains stationary while the fields are
delivered. Proton arc plans with optimized EL reduction settings were generated
for ten oropharyngeal cancer patients previously treated with IMPT. Proton arc
and clinical IMPT plans were compared in terms of integral dose and NTCP for
dysphagia and xerostomia, while target coverage was robust.
Results
Figure 1 illustrates the dependence of NTCP
and delivery time on number of ELs K and beams B. We found that 360 ELs
distributed over 30 beams generated proton arc plans with minimal NTCP. Relative
to corresponding IMPT plans, an average reduction of 21±3% in integral dose was
observed. The average NTCP for grade≥2 and grade≥3 xerostomia at six months
after treatment decreased with 4.7 ± 1.8% and 2.3 ± 0.8%, respectively, while
the average NTCP for grade≥2 and grade≥3 dysphagia decreased with 4.3 ± 2.9%
and 0.8 ± 0.4%, respectively. Figure 2 shows the expected reduction in NTCP per
patient, when proton arc therapy is employed.
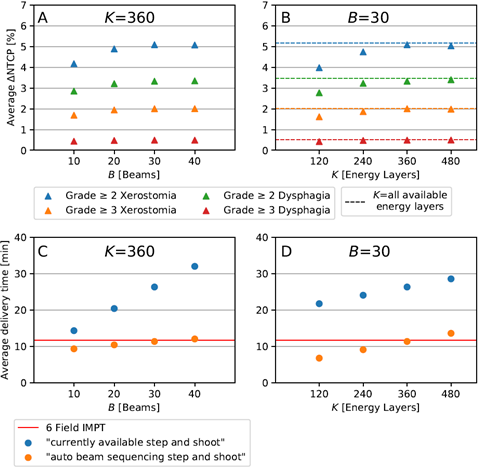
Figure [1]: The dependence of average reduction in plan toxicity with respect
to clinical IMPT plans (∆ NTCP), (graph A,B) and average estimated "step
and shoot" delivery time (graph C,D) on the number of beams B, in proton arc plans with 360 energy
layers (graph A,C) and on the number of energy layers K, in proton arc plans with 30 beams (graph B,D) for 3 oro-pharynx
patients. The dashed lines in gaph B represent the average ∆ NTCP when all
available enegy layers were used. The red line in graphs C and D show the
average delivery time for clinical 6 field IMPT.
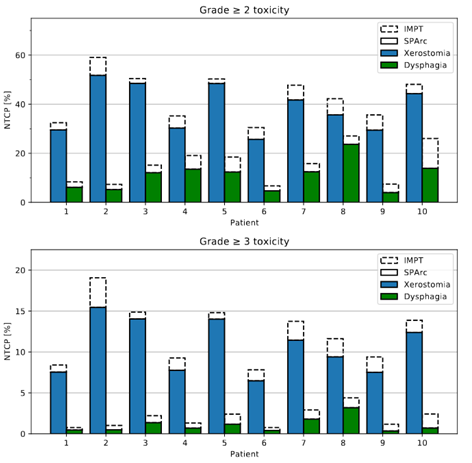
Figure [2]: NTCP
values at six months after treatment for grade≥2 toxicity (top) and grade≥3
toxicity (bottom) for clinical IMPT and proton arc plans employing 30 beams and
360 energy layers of 10 oropharyngeal patients.
Conclusion
Proton arc therapy demonstrates potential to further reduce toxicity relative
to clinical IMPT, especially when 360 ELs and 30 beams are employed for
oropharyngeal patients.