Model-based selection of NSCLC patients for proton therapy with heterogeneous dose distributions
OC-0450
Abstract
Model-based selection of NSCLC patients for proton therapy with heterogeneous dose distributions
Authors: Guido H.W. van Bogerijen1,2,3, Maria Fuglsang Jensen2, Mai Lykkegaard Ehmsen2, Lone Hoffmann3,4, Muhammad Shamshad2,3, Christina M. Lutz3, Marianne M. Knap3, Hanna R. Mortensen2, Ditte S. Møller3,4, Joost J.M.E. Nuyttens1
1Erasmus MC Cancer Institute, Department of Radiotherapy, Rotterdam, The Netherlands; 2Aarhus University Hospital, Danish Center for Particle Therapy, Aarhus, Denmark; 3Aarhus University Hospital, Department of Oncology, Aarhus, Denmark; 4Aarhus University Hospital, Faculty of Health Sciences, Aarhus University, Aarhus, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Proton therapy (PT) may reduce dose to organs at risk (OAR) compared to photon therapy (RT) when treating lung cancer patients, potentially resulting in less toxicity. Consequently, PT may better allow for dose escalation. We investigate these potential benefits in a planning study on locally advanced (LA)-NSCLC patients treated with heterogeneous dose distributions, with the purpose to select patients for whom PT is beneficial compared to conventional RT.
Material and Methods
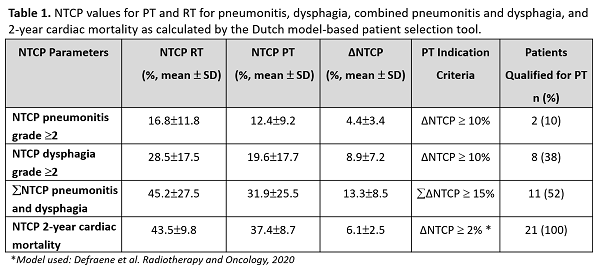
Twenty-one inoperable LA-NSCLC patients treated according to the HERAN trial (NCT03742687) with RT (IMRT) were retrospectively planned with PT. Fragile patients or patients with large tumor burden are treated with 50 Gy in 24 fractions to the CTV, but with a heterogeneous dose escalation of the primary tumor (GTV-T) and bulky lymph nodes (GTV-N high) up to mean doses of 66 Gy. PT plans were created with 2-4 beams with either SFO or MFO, using robust optimization (0 mm and 5 mm setup error; 4.5% range uncertainties) and required to fulfill V95%>99% for all CTVs, D1cc<60 Gy for esophagus and D0.05cc<50Gy for spinal cord. Plans were compared based on dose volume parameters and clinical parameters using the Dutch model-based patient selection tool. This tool uses 3 NTCP models selecting patients for PT if a ≥10% ΔNTCP for grade ≥2 pneumonitis or esophagitis, or ≥2% ΔNTCP for grade 4-5 cardiac toxicity between the PT and RT plan is found. The 3 models were externally validated within a large Dutch patient population. Comparison of plans was based on dose-volume parameters in target and OAR using paired t test. Clinical parameters were: smoking status, pulmonary comorbidity, GTV localization and volume, age, advent of chemotherapy, overall treatment time, and histology.
Results
Target coverage was adequate for all patients for PT and RT (all CTVs V95%>99%). Mean dose escalation was 65.5±0.3Gy vs. 64.8±1.6Gy (p=0.08) to GTV-T and 65.1±0.5Gy vs. 64.2±0.9Gy (p=0.09) to GTV-N high, respectively.
Mean doses to lungs (6.6±2.9Gy vs. 9.1±3.1Gy, p<0.001), esophagus (8.7±8.3Gy vs. 12.4±8.1Gy, p<0.001) and heart (2.5±2.4Gy vs. 6.3±4.6Gy, p<0.001) were significantly lower for PT compared to RT. ΔNTCP values for 1) pneumonitis showed: 10% of patients qualified for PT; 2) dysphagia: 38%, 3) pneumonitis and dysphagia: 52%, and 4) 2-year cardiac mortality: 100%. However, the result for five patients (patients 7, 10, 14, 17 and 19) qualifying for PT based on 2-year cardiac mortality was considered not clinically relevant, as the mean heart dose for these patients was low (<1Gy) for PT and RT. The patients with the largest combined ΔNTCP benefit (patients 8, 9, 11, 12 and 13) all had left-sided tumors at the heart level. (Fig 1, Table 1)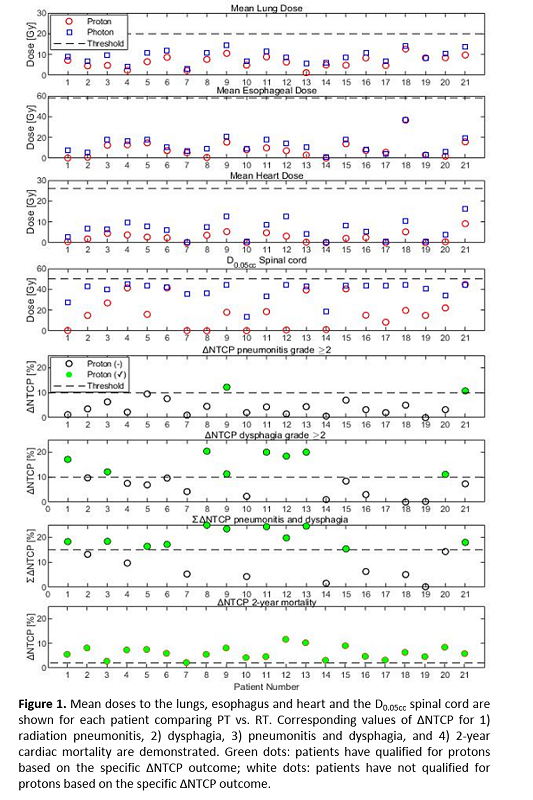
Conclusion
PT reduces dose to OAR compared to RT and may enable further dose escalation to the target. All NSCLC patients with heterogeneous dose distributions were model-based selected for PT. However, the patients benefiting the most from PT presented with left-sided tumors at the heart level.