First clinical experiences in treating oesophageal cancer with intensity-modulated proton therapy
Sabine Visser,
The Netherlands
OC-0947
Abstract
First clinical experiences in treating oesophageal cancer with intensity-modulated proton therapy
Authors: Sabine Visser1, Cássia O.Ribeiro1, Margriet Dieters1, Veronique E. Mul1, Anne Niezink1, Antje Knopf1,2, Johannes A. Langendijk1, Erik W. Korevaar1, Stefan Both1, Christina T. Muijs1
1UMCG, Radiotherapy, Groningen, The Netherlands; 2University Hospital of Cologne, Internal Medicine, Cologne, Germany
Show Affiliations
Hide Affiliations
Purpose or Objective
In oesophageal
cancer, less toxicity is expected when treating patients with intensity-modulated
proton therapy (IMPT) compared to volumetric modulated arc therapy (VMAT). In The
Netherlands, this complication risk reduction is estimated using multivariable
models and only patients who are expected to benefit clinically are selected
for IMPT. Due to the increased sensitivity to density changes of IMPT, there is a general concern of plan robustness. In this study, we
evaluated the first oesophageal cancer patients treated with IMPT in our clinic
in terms of target and organs-at-risk (OARs) dose robustness, as compared to
VMAT.
Material and Methods
For 20
consecutive oesophageal cancer patients, clinical IMPT and VMAT plans were
created on the averaged planning 4DCT. Weekly verification 4DCTs were acquired
to evaluate the robustness of target coverage over the course of IMPT and VMAT
treatments. If target coverage was degraded, replanning was performed and
evaluations were done for both the initial and the replan. Retrospectively,
target coverage was robustly evaluated for complete trajectories with and
without replanning, based on dose warping and accumulation. Three radiation
oncologists evaluated for each trajectory if accumulated target coverage was
sufficient. Accumulation was additionally performed using the nominal doses on
all repeated CTs for the adaptive IMPT and VMAT trajectories to evaluate the
treatment course mean lung dose (MLD) and mean heart dose (MHD). The accumulated MLD and MHD were then compared to the
planned dose to evaluate OARs dose robustness.
Results
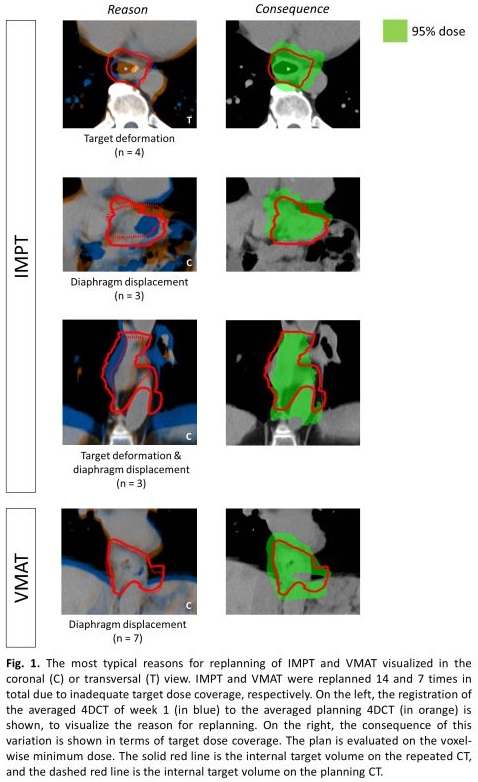
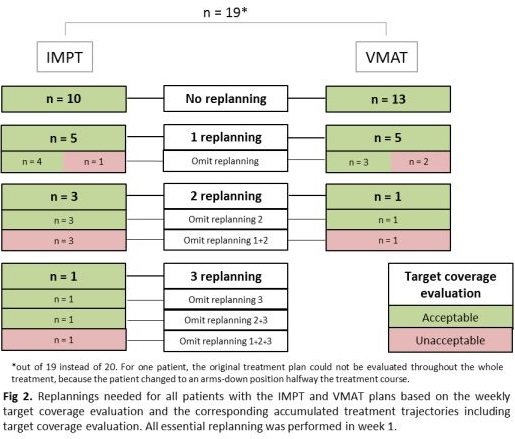
Replanning
was performed more often for IMPT (15x) than for VMAT (8x). For VMAT,
replanning was necessary only due to diaphragm displacements. Replanning for
IMPT was not always indicated for these cases, but IMPT suffered from other
variations like target deformations (Fig.1). Both adaptive treatment
trajectories resulted in adequate accumulated target dose coverage (Fig.2). Adaptation
after the first treatment week did not change the target coverage outcome.
Overall, replanning could have been omitted 9 times for IMPT and 4 times for VMAT
to still achieve an adequate accumulated target dose. Replanning in the first
week of treatment had the most clinical impact, as anatomical changes resulting
in insufficient accumulated target coverage were already observed at this
stage. No differences were found in MLD between the planned dose and the
accumulated dose. Accumulated MHD differed from the planned dose due to
variations in diaphragm position, but these differences were consistent between
IMPT and VMAT (mean MHD planning/accumulated 8.9 Gy/9.9 Gy [p>0.005] and
17.1 Gy/18.1 Gy [p<0.005], respectively).
Conclusion
Anatomical
changes in oesophageal cancer patients were already observed in the first
treatment week, affecting target and heart doses for both IMPT and VMAT. Adaptive
clinical workflows assured adequate target dose coverage over the course of
treatment.