Rapid IGRT-based proton dose estimation
OC-0946
Abstract
Rapid IGRT-based proton dose estimation
Authors: Stella Flampouri1, Mark McDonald1, William LePain1
1Emory University, Radiation Oncology, Atlanta, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
To develop and validate a rapid method to evaluate deviations of daily proton dose distribution from the planned within the timeframe of patient setup. Hypothesis: Dose changes can be predicted by stretching/contracting a reference dose of a single proton beam along its direction based on HU differences between a reference and a subsequent image.
Material and Methods
Reference dose is the plan dose calculated on a CT (pCT) and then associated with the reference CBCT (refCBCT). RefCBCT is the 1st-day CBCT deformed to the anatomy of the pCT. Along a beam path, cumulative HU values are recorded for refCBCT and a daily CBCT (CBCTi). Dose from the refCBCT is then stretched or contracted based on the difference of cumulative values. Prior, refCBCT and CBCTi are smoothed to lessen noise and image artifacts. The images are also crudely corrected for the shape of the HU-to-RSP curve by first using HU histogram matching between pCT and refCBCT and then applying the CT calibration curve. This correction is inaccurate for actual dose calculation on a CBCT, but its effectiveness for comparison between two CBCTs was investigated. Finally, the 1D-warped beam doses are summed into total fractional dose. To validate the method for bilateral HN we compared the estimated fractional doses with our clinical off-line standard. This includes deforming the closest in time available CT (pCT or QACT) to CBCTi to create a synthetic CT (sCTi) and then use that to calculate dose in the treatment planning system with Monte Carlo. Dose on CTBTi and sCTi was compared with Gamma-index (3mm/3%). 21 oropharyngeal patients previously treated with bilateral neck proton radiation were selected for validation. Patients had at least 3 QACTs and weekly CBCTs (in total 97 CBCTs and 78 QACTs).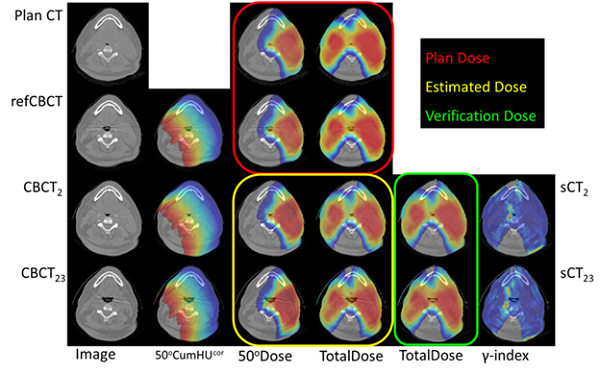
Results
Variations of CBCT corrections such as image smoothing, HU histogram matching and application of approximate calibration curves were applied in various combinations. The gamma-index for calculated dose on sCTs versus predicted dose on matching CBCTs acquired 35 days post simulation for all 21 patients was obtained for different levels of corrections. Application of a calibration curve was the only significant correction. Additional corrections improved the agreement but the difference was not statistically significant. The accuracy of the method decreased with increased number of days past simulation. For all 21 patients we compared the predicted dose on 97 CBCTs with calculated dose on matching sCTs. The mean gamma-index pass rate was 98.2% (σ = 2.5%). The 3 lowest rates (<95%) belonged to the same patient with severe dental artifact. Duration of CBCT-based dose prediction was recorded, on average it takes 29s (σ = 4.5s). That includes reading the daily CBCT, correcting the HU, stretching/compressing dose for 5 beams and summing them up.
Conclusion
Using HU-based dose deformation along a proton beam, a rapid and accurate fractional dose estimate for oropharyngeal radiation was obtained and could be used for real-time guidance.