Adaptive fractionation at the MR-Linac based on a dynamic programming approach
Yoel Samuel Pérez Haas,
Switzerland
OC-0944
Abstract
Adaptive fractionation at the MR-Linac based on a dynamic programming approach
Authors: Yoel Samuel Pérez Haas1, Roman Ludwig1, Riccardo Dal Bello1, Lan Wenhong1, Stephanie Tanadini-Lang1, Jan Unkelbach1
1University hospital Zurich, Radiation Oncology, Zürich, Switzerland
Show Affiliations
Hide Affiliations
Purpose or Objective
Inter-fraction
motion of tumors and dose-limiting OARs can be visualized using MR guidance.
Whereas standard treatments deliver the same dose in each fraction, adaptive
fractionation (AF) is an approach to exploit inter-fraction motion by
increasing the dose on days when the distance of tumor and OAR is large and
decreasing the dose on unfavorable days. We develop an algorithm for AF and
evaluate the concept for former patients treated at the MR-Linac for abdominal
tumors in 5 fractions.
Material and Methods
Given
daily MR scans and adaptive treatment plans, inter-fractional changes in
fraction t are quantified by sparing factors δt, which
are defined as the ratio of dose delivered to the OAR (D1cc) and the
tumor (D95%). The key problem of AF is to decide on the dose to
deliver in fraction t, given today's δt and the dose
delivered in previous fractions, but with unknown future δs. This
problem can be formulated as a Markov decision problem and solved with a
dynamic programming algorithm. The algorithm assumes a normal distribution over
δ with mean and variance estimated from previously observed patient-specific
δs and a population based prior for the variance. Based on the
distribution, the algorithm computes optimal doses that maximize the expected
tumor BED10 while staying below the maximum BED3 of 90 Gy
in the OAR (30 Gy in 5 fractions). To evaluate the algorithm, 10 MR-Linac
patients were exported in whom tumor dose was compromised due to proximity of
bowel, stomach, duodenum or heart. Moreover, 1000 synthetic patients with
similar δ distribution have been sampled. AF was compared to a standard plan
which delivers 6 Gy to the OAR in each fraction to reach exactly the 90 Gy BED3
constraint.
Results
In
7 of the 10 patients, AF was equal or increased the tumor BED10, on
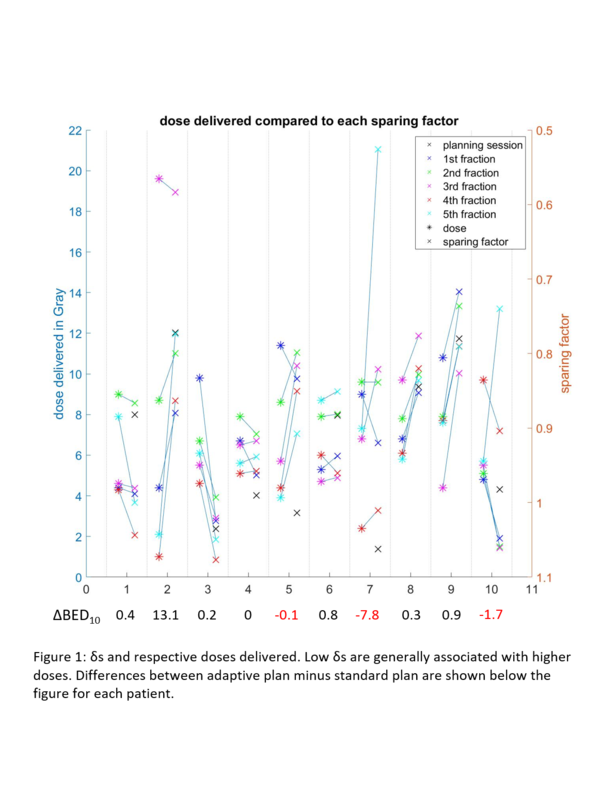
average by 0.72 Gy (1.2%). Figure 1 shows the δ's and the respective doses based on AF for all
patients. The biggest increase of 13.1 Gy (18.4%) was achieved for patient 2
with δ=[0.88,0.8,0.58,0.86,0.77] where AF delivered tumor doses of
[4.4,8.7,17,0.9,2.1] and thereby exploited the low δ in fraction 3.
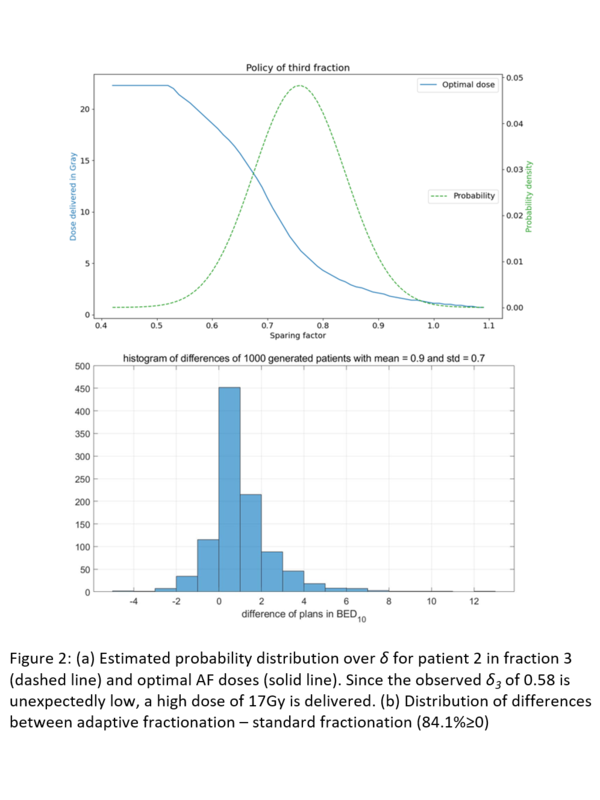
Figure 2a) illustrates the optimal policy for fraction 3, i.e. optimal dose to
deliver as a function of δ. For the 1000 generated patients, 84.1% of
plans were equal or superior to the standard plan with a mean improvement of
1.01 Gy (1.5%) BED10. A distribution of the differences is shown in
Figure 2b). With the most extreme plans having a benefit of up to 12 Gy BED10.
Conclusion
On average, AF provided only a small increase in tumor
BED. However, AF may yield substantial benefits for individual patients with
large variations in the geometry.