Reirradiation of pediatric patients with diffuse midline glioma
Daniella Elisabet Østergaard,
Denmark
OC-0761
Abstract
Reirradiation of pediatric patients with diffuse midline glioma
Authors: Daniella Østergaard1, Ivan Richter Vogelius2, Rene Mathiasen3, Karsten Nysom4, Morten Jørgensen1, Astrid Marie Sehested4, Maja Maraldo1
1Rigshospitalet, Section of Radiotherapy, Department of Oncology, Copenhagen, Denmark; 2Rigshospitalet/ Copenhagen University, Section of Radiotherapy, Department of Oncology/2Faculty of Health and Medical Sciences, Copenhagen, Denmark; 3Rigshospitalet, Department of Pediatrics and Adolescent Medicine, Copenhagen, Denmark; 4Rigshospitalet, 3Department of Pediatrics and Adolescent Medicine, Copenhagen, Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Diffuse midline glioma (DMG) is a primary
brain tumor seen mainly in children. Following radiotherapy, the only
well-documented life-prolonging therapy, the median survival is still only 11
months from diagnosis of DMG. Over the last decade, re-irradiation (reRT) at
relapse has been increasingly used, showing a longer survival and symptom palliation
with limited toxicity. ReRT of DMG at relapse is, however, not yet consistently
considered standard of care throughout Europe. We reviewed
our institution’s experience with reRT of DMG including the site of relapse and
the cumulated dose to organs at risk (OAR).
Material and Methods
We reviewed the baseline and
treatment characteristics of all patients with DMG receiving reRT from June 2011
to June 2021. Information was obtained through national electronic health
records following ethical permission. For each patient, the initial and re-irradiation
RT plans were visually assessed to evaluate any possible overlap between the
two treatments. The cumulative dose to OAR were calculated as EQD2 = D((d + α/β)/(2 + α/β)), with α/β=2Gy for neurological tissue based on the published literature. Records
were scanned for early toxicities 6 weeks following start of reRT.
Results
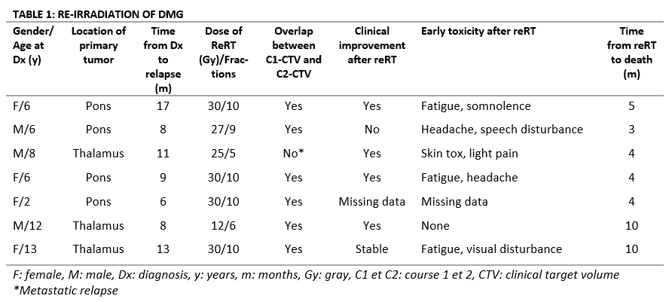
Among
19 children from East Denmark irradiated for DMG, seven received reRT (Table 1).
Their median age at diagnosis was six years (range, 2-13) and their median
overall survival was 20 months (9-30). The median time from initial RT to reRT
was 10 months (8-17) and the median time from reRT to death was 4 months (3-10).
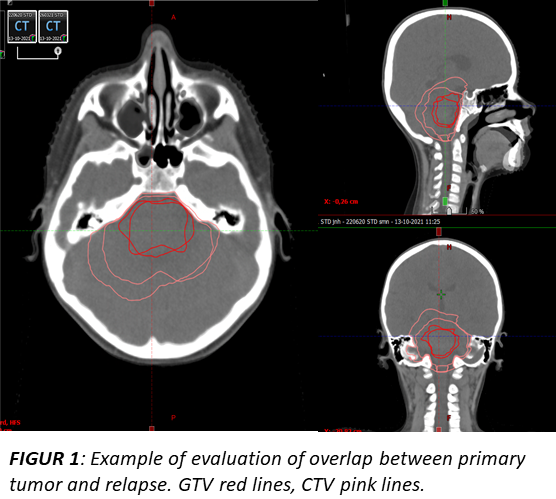
For six patients, the relapse overlapped with the localization of the primary
tumor (Figure 1) and the cumulated doses to surrounding tissue was calculated. The
median cumulated dose to the chiasm was 64 Gy (range, 37-85.), to the left and
right optic nerve 20 Gy (10-24) and 23 Gy (11-33), respectively, and to left
and right hippocampi 53 Gy (37-87 ) and 53 Gy (37-86), respectively. All but
one patient (missing data) had improved or stabilized symptoms from both
courses of RT. Early toxicities following reRT were described as minor, only managed
with basic supportive care and, for two patients, no toxicity was reported at
all. No patients were diagnosed with clinically significant radionecrosis.
Conclusion
Our data support reRT as a relevant palliative treatment for children
with DMG. Despite the overlap
of treatment fields,
there was no reported excessive early toxicity. Due to the limited survival time of patients, palliation with minimal toxicity and
high quality of life should be considered standard of care. Further studies are
needed to define the optimal population for reRT of DMG.