Fifty-two patients were included in the study: median age at RT was 5.6 (range, 0.9-30.3) years, median RT dose was 40Gy. At RIM diagnosis, median age was 33.9 (range, 13.8-54.1) years, with median latency period of 25.5 (range, 8.8-53.2) years. 37% of patients had multifocal RIM. 88% of patients were asymptomatic at presentation.
A total of 87 RIM were identified. Median follow-up was 11 years. RIM location was convexity (48%), falcine/tentorial (34%), basal (16%), and spinal (2%). Initial RIM management was active surveillance (77%), upfront surgery (21%), SRS (1%), chemotherapy (1%).
Active surveillance was adopted for 67 RIM in 40 patients. Of these patients, 82.5% had RIM diagnosed on MRI screening. At 10 years, the cumulative actuarial incidence of surgery for initially surveilled RIM was 21% (95%CI, 12%-31%). The most common indication for surgery was asymptomatic tumour growth (62.5%). Neurological sequelae due to RIM progression was reported in 2 (5%) patients on active surveillance.
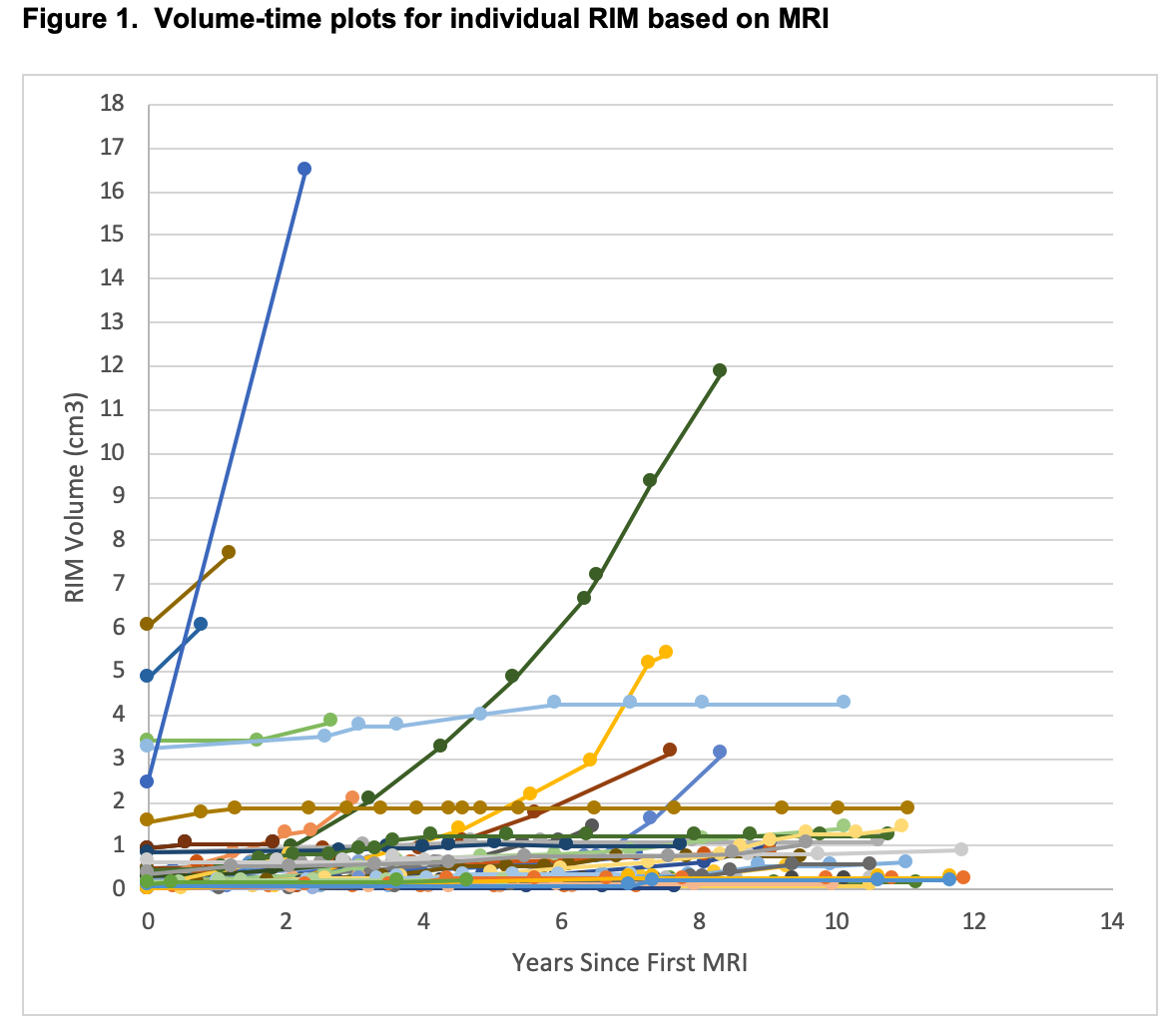
MRI data was available for 61 (91%) RIM on active surveillance. Mean tumour volume at diagnosis was 0.53cm3 (SD=1.14). Median absolute growth rate was 0.05cm3/year (IQR 0.01-0.11); median relative growth rate was 26% per year (IQR 7-79). Radiological growth pattern of individual RIM is shown in Figure 1.
Resection was performed for 33 RIM (30 patients), 54.5% at diagnosis and 45.5% after active surveillance. Pathological grade was WHO Grade I (85.2%), II (11.1%), III (3.7%). Gross total resection was achieved in 79%. Following resection, actuarial 10-year local recurrence rate was 12% (95%CI: 3-29).
There were 8 deaths: 1 due to RIM. OS was 88% (95%CI, 74%-95%) at 10 years.