ESTRO-Jack Fowler University of Wisconsin Award: Sources of errors in radiotherapy as assessed with the IROC lung, H&N and spine phantoms
Sharbacha Edward,
USA
OC-0290
Abstract
Sources of errors in radiotherapy as assessed with the IROC lung, H&N and Spine phantoms
Authors: Sharbacha Edward1, Christine Peterson2, Rebecca Howell3, Peter Balter3, Julianne Pollard-Larkin3, Stephen Kry3
1MD Anderson Cancer Center, Radiation Physics, Houston, USA; 2MD Anderson Cancer Center, Biostatistics, Houston, TX, USA; 3MD Anderson Cancer Center, Radiation Physics, Houston, TX, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
Phantoms from the
Imaging and Radiation Oncology Core (IROC) show 8-17% of institutions fail to
deliver the intended dose within established criteria. This work sought to
quantify the source and magnitude of various sources of error in treatment delivery.
Material and Methods
IROC lung (n = 41), head and neck
(H&N) (n = 36) and spine (n = 63) phantoms irradiated by various institutions,
as an end-to-end radiotherapy test, were evaluated for quantifiable errors that may occur in the planning and
delivery phases of treatment. Plans were independently recalculated to assess
dose calculation errors, delivery log files were used to evaluate delivery
errors, and contemporaneously conducted beam output audits were used to
evaluate machine output errors.
The errors from each source were used to characterize the dose
deviations that exist between the institution’s TPS dose and measured TLD dose,
to determine how much of that deviation was accounted for by the error sources
investigated. A dose difference metric, D, was
used to describe the result, where a positive D value indicated the presence of
true error, and a negative D value did not.
Phantom results were evaluated in 2
groups, separated by a threshold total dose deviation (3.2%) (Kirby, 1992) to account for measurement uncertainty in phantom TLD doses.
No delivery error was assessed for spine due to lack of log file data.
Results
Among all 3 phantoms, cases with absolute
dose deviation within measurement uncertainty (< 3.2%), expectedly had a negative
average D value, showing that not much, if any, of the error could be described
by the categories investigated.
Phantom results with substantial dose
deviation (> 3.2%) had positive D values in all categories, indicating that some
of the existing dose deviations were accounted for by the error modes we
evaluated. Output error was the largest category of error for the lung phantom (16%),
whereas dose calculation error was the major contributor for the H&N (49%)
and spine (40%). The total magnitude of error quantified among these phantoms, i.e.,
the % of absolute dose deviation accounted for, was 20.5%, 68.3% and 70.9% for lung,
H&N, and spine respectively (Fig. 1). These findings were further emphasized
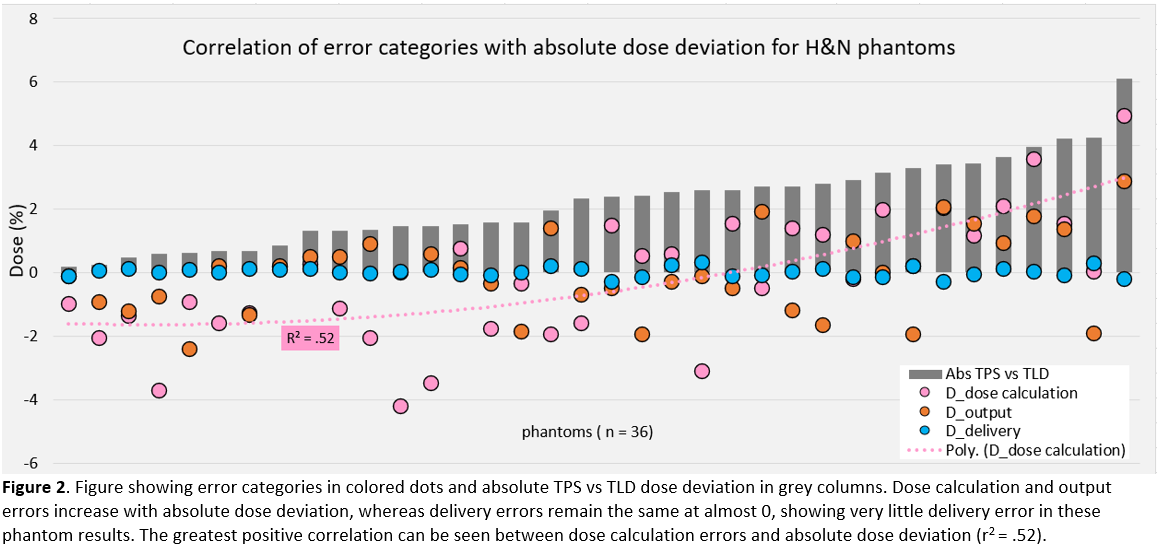
by the positive correlations found between absolute dose deviation and error
type per phantom: lung = output (Pearson correlation; r = .54, p < .01),
H&N = dose calculation (r = .72, p < .01) (Fig. 2), spine = dose
calculation (r = .59, p < .01).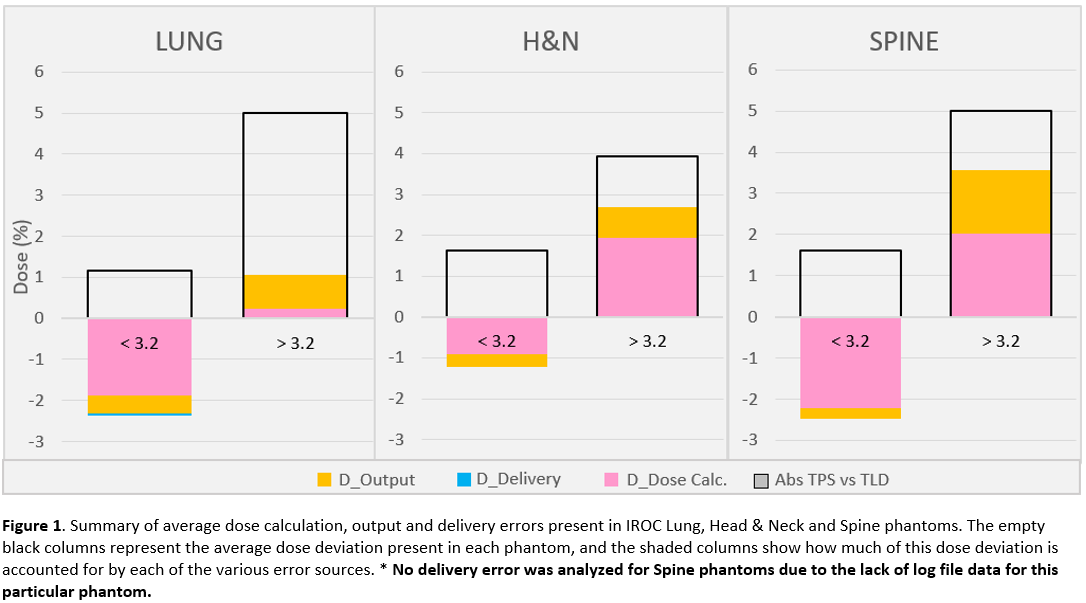
Conclusion
Errors in radiotherapy remain prevalent and require
attention and resolution in the community. For phantom results with
non-negligible dose deviation, we identified 20.5%, 68.3% and 70.9 % of errors
for the lung, H&N, and spine phantom respectively. Dose calculation and
machine output errors both contributed substantially to the phantom error. As
these are common sources of error, the radiation oncology community should pay
particular attention to them.