Dosimetric evaluation of dose calculation uncertainties for MR-only treatments of pelvic MRgRT
OC-0289
Abstract
Dosimetric evaluation of dose calculation uncertainties for MR-only treatments of pelvic MRgRT
Authors: Ivan Coric1, Kumar Shrestha2, Thais Roque2, Nikos Paragios2,4, Daniel Zips3, Daniela Thorwarth1, Marcel Nachbar1
1University Hospital and Medical Faculty. Eberhard Karls University Tübingen, Department of Radiation Oncology, Section for Biomedical Physics, Tübingen, Germany; 2TheraPanacea, TheraPanacea, Paris, France; 3University Hospital and Medical Faculty. Eberhard Karls University Tübingen., Department of Radiation Oncology, Tübingen, Germany; 4CentraleSupelec, University of Paris-Saclay, Gif-sur-Yvette, France
Show Affiliations
Hide Affiliations
Purpose or Objective
MR-guided radiotherapy (MRgRT) allows plan adaptation on the MRI of the day. However, the current workflow for the 1.5 T MR-Linac (Elekta AB, Stockholm, Sweden) employs a structure specific bulk electron density (ED) overwrite derived from a planning CT for dose calculation. This workflow does not only introduce uncertainties due to assignment of mean EDs, but still requires a planning CT. In this work, we investigated the uncertainty of the current patient specific (PSCT) dose calculation in contrast to the correct calculation on a CT and compared to MR-only workflows using population based bulk ED (PBCT) and artificial generative adversarial neural networks (GANs) intelligence-based generated pseudo CTs (AICT).
Material and Methods
Ten primary prostate cancer patients treated on the MR-Linac were chosen, based on best visual congruence between the planning CT and daily MRI. Treatment plans (20x3Gy) were optimized on the planning CT with the clinical TPS (Monaco 5.4). The CT dose distribution was then compared to the different synthetic CT approaches. (1) For PSCT, mean ED for femur, pelvis, sacrum, rectum, bladder, and patient were assigned based on mean CT densities. (2) Population-based mean EDs were derived based on 50 recent patient datasets and assigned to the structures for the PBCT approach. (3) A pseudo-CT AI-model was generated using end-to-end ensembled self-supervised GANs endowed with cycle consistency on a dataset of 42 patient with each one planning CTs and in average 5 T2w-MRIs. This model was used to create AICTs of the T2w-MRIs for dose calculation. For the analysis the planning CT was registered to the MRI, structures rigidly propagated, and the treatment plan recalculated on the correlating isocenter. For an evaluation differences in DVH-parameters were analyzed and dose distributions compared with global gamma criteria.
Results
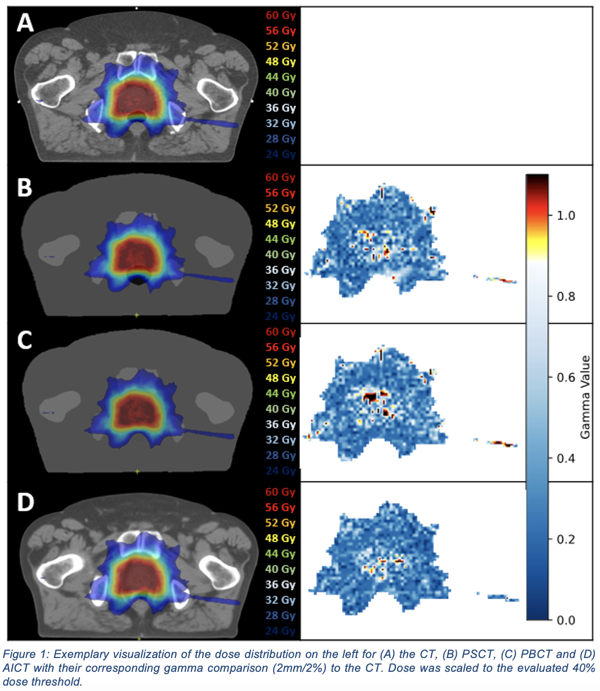
All three approaches reproduced for all patients the dose distribution based on a gamma criterion of 3mm/3% (40% threshold) with a pass rate greater than 98%. On a 2mm/2% criterion (40% threshold) a mean gamma pass rate for PSCT, PBCT and AICT of 96.53%, 96.32% and 96.9% was present (Fig. 1).
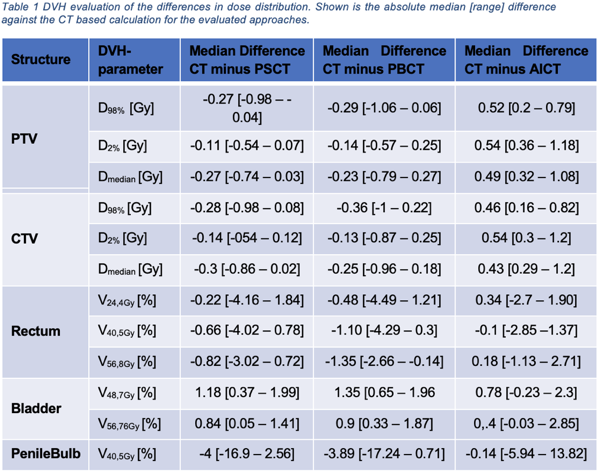
The same is observed in terms of DVH-parameters (cf. table 1). Whilst the PTV/CTV parameters were better reproduced by the bulk density approach, differences for OARs were smaller for the AICT.
Conclusion
We presented a detailed analysis of uncertainties of pCT concepts for pelvic MRgRT. The current workflow depicts dose uncertainties based on bulk density approaches. Both a PBCT and AICT approaches, which bypass the need for a planning CT, might be considered clinically acceptable whilst reducing imaging dose and registration issues. Especially for air influenced OARs the AI-based pseudo-CT generation approach shows a better performance by more accurately predicting the different density gradients.