From PTV-based planning to robust planning: external validation of a robustness evaluation approach
Roel Kierkels,
The Netherlands
OC-0286
Abstract
From PTV-based planning to robust planning: external validation of a robustness evaluation approach
Authors: Roel Kierkels1, André Minken1, Erik W. Korevaar2
1Radiotherapiegroep, Department of radiation oncology, Arnhem/Deventer, The Netherlands; 2University of Groningen, University medical center Groningen, Department of radiation oncology, Groningen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
The traditional planning target volume (PTV) accounts for systematic and random treatment (e.g. setup) uncertainties, but assumes a static dose cloud approximation, that does not hold in areas with high density variations in both photon and proton treatments. In contrast, robust planning algorithms mathematically account for errors during plan optimization, but cannot rely on the traditional PTV-based plan evaluation anymore. Therefore, Korevaar et al. (1) proposed an alternative plan evaluation method, using voxel-wise minimum/maximum (vw-min/max) dose distributions. They calibrated the traditional PTV D98%≥95% with -0.9% and D2%≤107% with 2.3% on average for all tumor sites. The proposed plan evaluation method was validated in another radiotherapy institute and calibrated for various treatment sites to determine target criteria when PTV-based planning is replaced by robust planning. We hypothesized that sampling regular or random setup error directions to create the required vw-min/max dose distributions does not influence the results.
Material and Methods
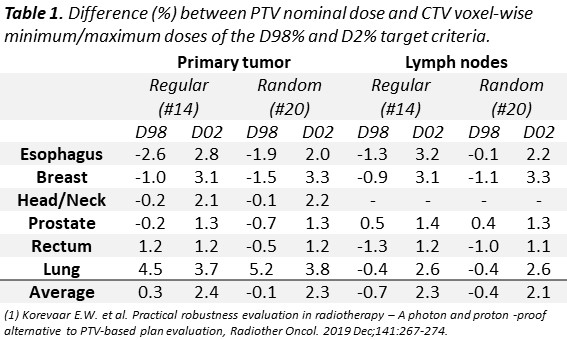
The D98% and D2% of intensity modulated photon plans of (in total 294) lung, breast, esophagus, rectum, prostate, and head and neck cancer patients were retrospectively evaluated on the PTV of the nominal dose distribution and the clinical target volume (CTV) of the vw-min/max dose distribution. The vw-min/max dose distributions were created from a combination of 14 perturbed dose distributions. The perturbed error scenarios were drawn from the cardinal axis and the corners of a cube, projected on a sphere with a magnitude of shift equal to the CTV-PTV margin. Similarly, the vw-min/max dose distributions were constructed from 20 randomly sampled perturbed scenarios on the same sphere. The PTV D98%/D2% and the CTV D98%vw-min/D2%vw-max were compared and calibrated for each tumor site.
Results
On average, the primary CTV D98%vw-min≥95% was highly correlated with the PTV D98% (R2=0.99, slope=1.0), whereas the D2%≤107% required a +2.4% correction for robust CTV evaluation (i.e. D2%vw-max≤109.4%). Site specific evaluation showed that the primary CTV D98%vw-min≥95%/D2%vw-max≤107% required a correction of -2.6%/2.8% (esophagus), -1.0%/3.1% (breast), -0.2%/2.1% (head and neck), -0.2%/1.3% (prostate), 1.2%/1.2% (rectum), and 4.5%/3.7% (lung) using regularly distributed scenario directions. On average, the correction for the D98% CTV nodes was -0.7%. The results of the regular and random sampling evaluation were on average within 0.4% and varied per tumor site with 0.2%, on average (table 1).
Conclusion
A clinical plan robustness evaluation method using vw-min/max dose distributions can replace traditional PTV-based plan evaluation when robust planning is introduced. We externally validated and calibrated the method and the average results for PTV D98% and D107% were, as compared to the results of Korevaar et al., within 0.5% and 0.1% , respectively. Differences in sampling method (regular or random) were negligible.