Identification of dose rate transients at the start of every beam-on period for a gated MR-linac
Mads Fjelbro Klavsen,
Denmark
OC-0280
Abstract
Identification of dose rate transients at the start of every beam-on period for a gated MR-linac
Authors: Mads Fjelbro Klavsen1, Kristian Boye2, Rasmus Hvass Hansen2, Ivan R. Vogelius2, Claus P. Behrens3, Christina Ankjærgaard1, Claus E. Andersen1
1Technical University of Denmark, Department of Health Technology, Roskilde, Denmark; 2Copenhagen University Hospital – Rigshospitalet, Dept. of Oncology, Copenhagen , Denmark; 3Copenhagen University Hospital – Herlev and Gentofte, Dept. of Oncology, Copenhagen , Denmark
Show Affiliations
Hide Affiliations
Purpose or Objective
Some MR-linacs have the ability to perform
gated treatments based on continuous tracking on 2D images acquired during dose
delivery (ciné). This potentially reduces the treatment margins required for
tumor coverage, but at the same time adds complexity to the dosimetric QA. To characterize
the gating performance of a MR-linac with respect to dose, we have developed a dosimetry
system with dose-per-pulse time resolution that can be used without distorting
the MR images. The system is based on one or more plastic scintillation point detectors
(PSD) coupled to optical PMMA fibers. This all-plastic system has a high degree
of water equivalence. In this work, the system was applied on the Viewray
MRIdian 0.35 T MR-linac and was able to identify a systematic transient in dose
rate at the start of every beam-on period.
Material and Methods
The PSD in this study was a BCF-60
scintillator coupled to a 15 m long 1 mm diameter PMMA optical fiber connected
to the readout equipment (ME40, DTU). The PSD was placed in a water-filled
plastic tube that was inserted into a dynamic MRI compatible phantom (CIRS, US).
To avoid large dose gradients near the penumbra region, the PSD was placed at
the beam axis and irradiated with a 20 cm x 14 cm field. The
piston of the CIRS phantom performed a sinusoidal movement with a period of 4 s
and an amplitude of 12.83 mm. The gating window boundary was set ±
5 mm from the center of the sinusoidal movement. Figure
[1] shows the three different gating phases of a half sinusoidal cycle (the piston position in the lower
panel corresponds the red part of the motion curve).
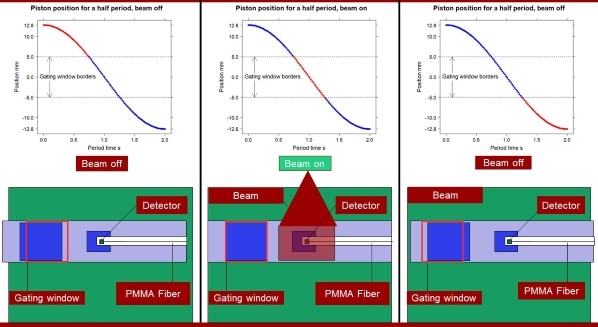
Figure [1]
Results
Due to the high time resolution of the detector
system, it was possible to identify two different transient (warm-up) effects
in the MRIdian. The first was a reduced dose rate during the initial part of every
gating event when the beam turned on. The reductions were up to 10 % of the
final (stable) dose rate. The transients gradually decreased with time and
vanished completely after 1.5 s or less.
The second effect was a slow but systematic increase of the measured
dose rate, at the reference point, of about 2% throughout the whole treatment (figure
[2]). Finally, a latency of the gating mechanism was observed resulting in dose
delivery even when the piston was outside the gating area. This most likely reflected the
limited frame rate (4 fps) used in this treatment.
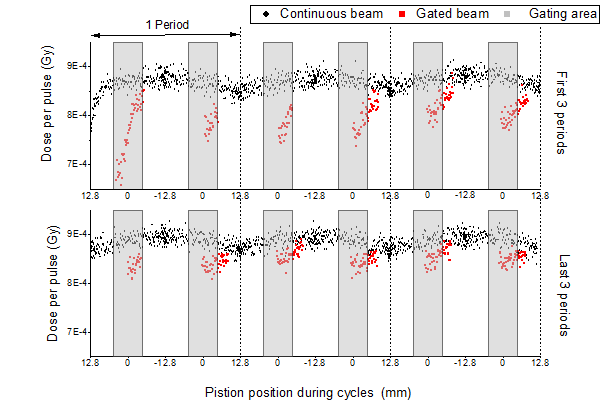 Figure [2]
Figure [2]
Conclusion
The dose-per-pulse scintillator system
revealed temporal effects in the MRIdian beam gating system using.
The most significant being the systematic transient each time the beam was
turned on (up to 10% reduction compared to the final dose rate). It is unknown whether
this phenomenon is specific for the accelerator tested. Furthermore, the
clinical relevance of these effects is not known and are likely depending on
the exact gating procedure. For challenging cases with low duty cycle it should
be considered to what extend warm-up or latency effects could perturb the delivered
dose.