Standard vs dose escalated chemoradiotherapy in anal cancer: Phase II results of the PLATO-ACT5 RCT
OC-0269
Abstract
Standard vs dose escalated chemoradiotherapy in anal cancer: Phase II results of the PLATO-ACT5 RCT
Authors: Alexandra Gilbert1, Joanne Webster1, Sarah Brown1, Joanne Copeland1, Sharon Ruddock1, Richard Adams2, Mark Harrison3, Rebecca Muirhead4, Andrew Renehan5, David Sebag-Montefiore1, Maria Hawkins6
1University of Leeds, Leeds Institute of Clinical Trials Research, Leeds, United Kingdom; 2University of Cardiff, Cardiff University Department of Cancer and Genetics and Velindre Hospital, Cardiff, United Kingdom; 3Mount Vernon Hospital, Mount Vernon Centre for Cancer Treatment, London, United Kingdom; 4Oxford University Hospitals NHS Trust, Department of Oncology, Oxford, United Kingdom; 5University of Manchester, Division of Cancer Sciences, Manchester, United Kingdom; 6University College London, Dept of Medical Physics & Biomedical Engineering, London, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
The optimal dose of radiation for advanced anal cancer is uncertain. ACT 5 is a phase II/III prospective, multi-centre, open-label randomised 3-arm trial investigating dose escalated intensity modulated radiotherapy (IMRT) with concomitant chemotherapy in locally advanced disease. It is part of the PLATO trial platform. The primary phase III outcome is 3-year locoregional control. We report the phase II results of treatment compliance, acute toxicity up to 3-months and patient reported outcomes (PROs) up to 6-weeks on the first 140 patients (pts).
Material and Methods
Pts with T2N1-3M0, or T3-4 Nany M0 squamous cancer of the anus received 28 fractions (F) of IMRT at total standard dose of 53.2Gy or escalated to 58.8Gy or 61.6Gy to the gross tumour (elective nodal irradiation 40Gy in 28F in all arms) with concurrent mitomycin 12mg/m2 day 1 and capecitabine (CAP) 825mg/m2 twice daily (week days) or 5-flurouracil 1000mg/m2 days 1-4 and 29-32 (centre choice). The phase II primary endpoint was ≥ Grade 3 (G3) neutropenia during treatment, to determine the most suitable arm to continue to phase III. 140 patients were required to exclude an unacceptable rate of ≥60% with a targeted rate of <40% in each of the dose escalated arms. Compliance to RT (no delay >3 days due to toxicity) and chemotherapy, worst acute toxicity up to 3-months (CTCAEv5) and a priori selected PRO items up to 6-weeks (EORTC-QLQ C30 and ANL27) were analysed. Recruitment to the phase III component of the trial is continuing.
Results
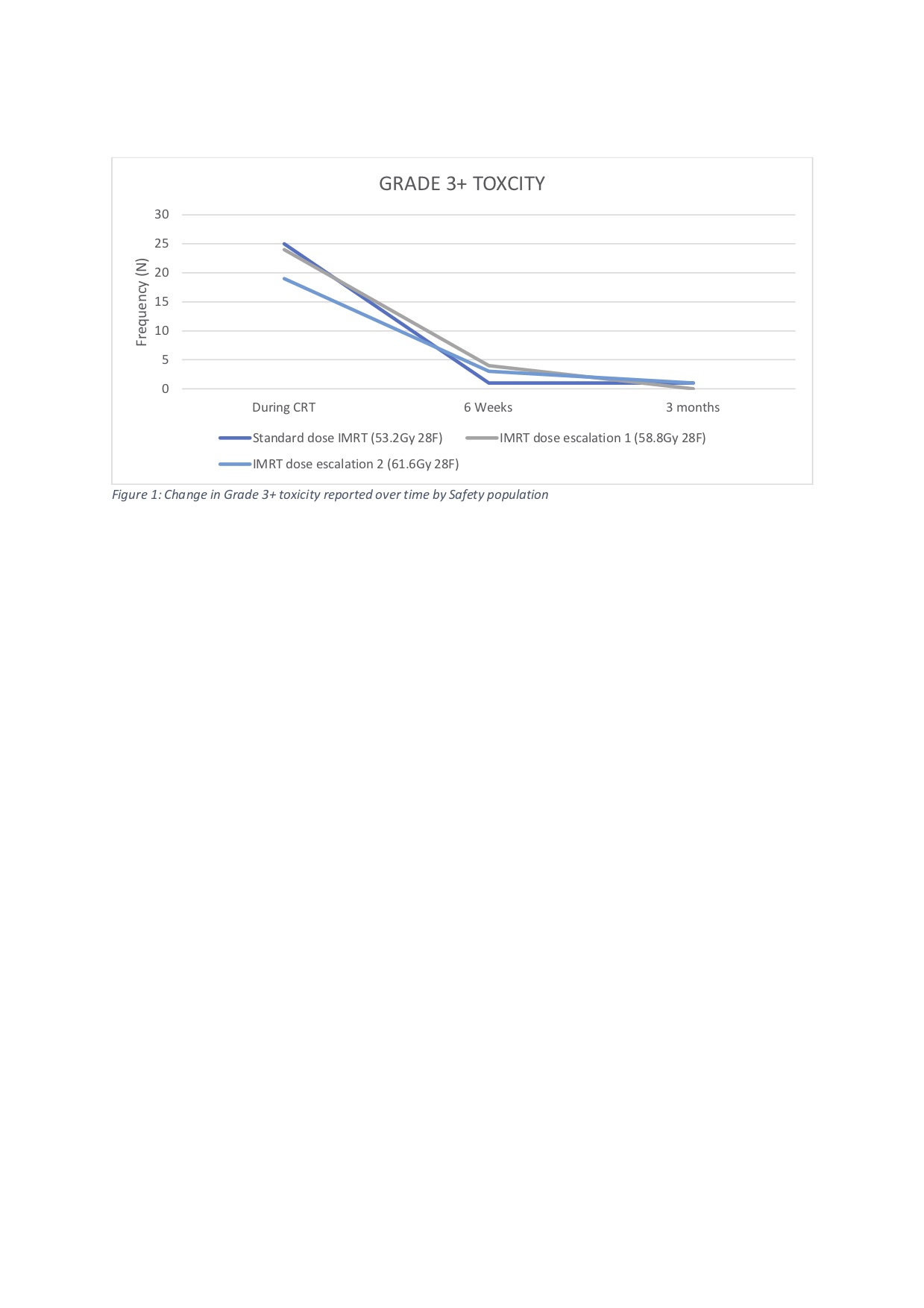
140 pts were enrolled from 36 UK sites (53.2Gy n=47; 58.8Gy n=47; 61.6Gy n=46) and completed 6-month follow up. 79% female, median age 60 years (36-77), T2 35%, T3 36%, T4 29% and N+ 81%. All pts received planned RT dose with only 1 patient (61.6Gy) completing >43 days due to haematological toxicity. 43 pts (31%) experienced at least one interruption to their radiotherapy (53.2Gy n=14; 58.8Gy n=16; 61.6Gy n=13). Chemotherapy (5FU n=44; CAP n=96) modifications were in the majority of cases due to toxicity (72.1%): reductions (CAP n=3; 5FU n=4), temporary omissions (CAP n=33, range 1-21 days; 5FU n=4); delays (CAP n=4; 5FU n=4). During CRT 68 patients (49%) reported ≥G3 acute toxicity (53.2Gy n=25; 58.8Gy n=24; 61.6Gy n=19). ≥G3 neutropenia rates were low and comparable across treatment arms (Overall n=10; 7%; 53.2Gy n=3; 58.8Gy n=3; 61.6Gy n=4). 28% reported ≥G3 radiation dermatitis and 7% ≥G3 diarrhoea. At 6-weeks and 3-months post CRT ≥G3 toxicity rates monotonically decreased in all arms (n=76; see figure & table). Pre-specified PRO items on quality of life, pain, and bowel toxicity were worst in final treatment week, with most items improving to baseline or better levels by 6 weeks with no differences between arms observed. 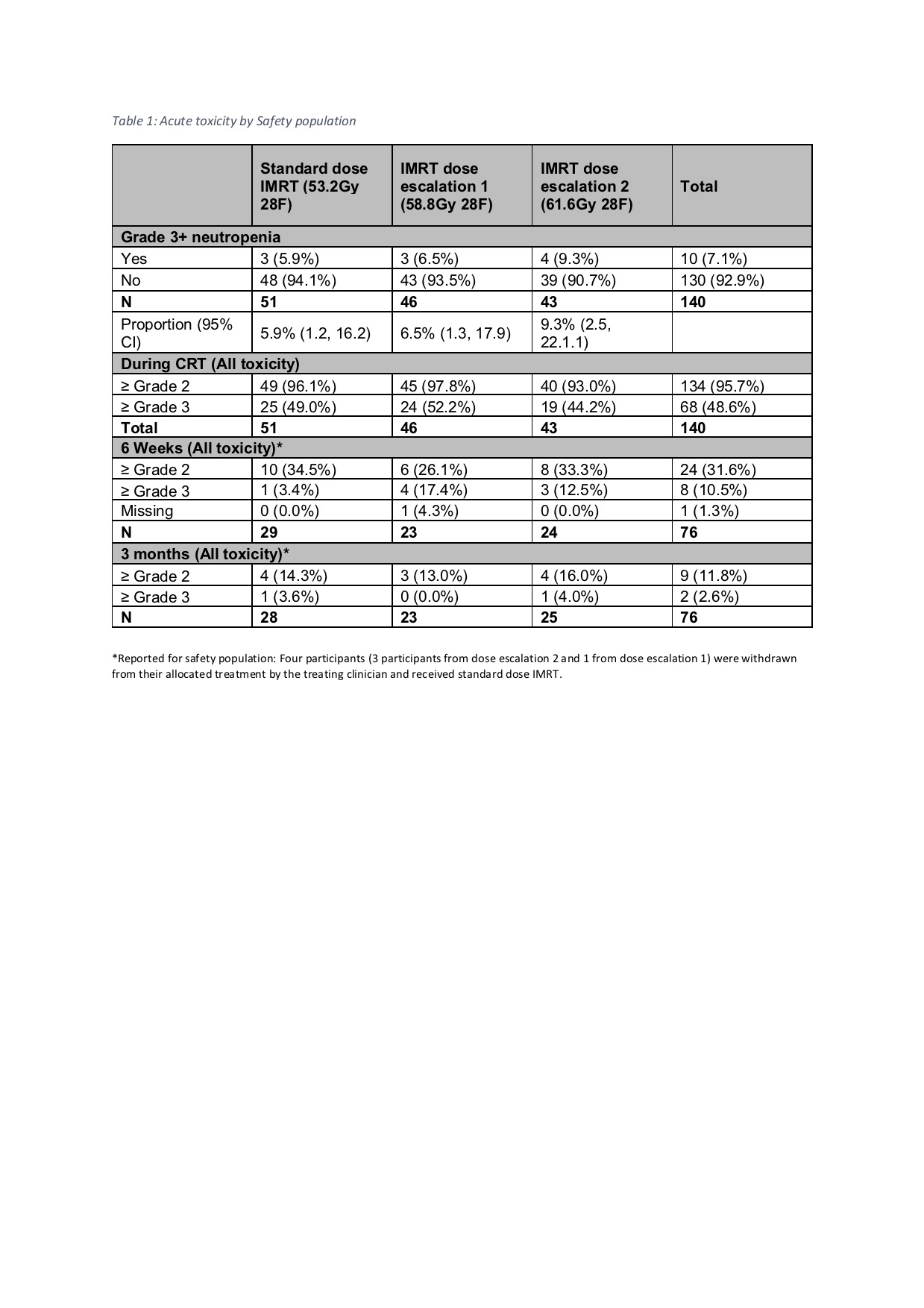
Conclusion
The phase II target was achieved with early safety data showing acceptable acute toxicity, compliance, and PROs with IMRT dose intensification. Both escalation arms have been taken forward into phase III. Recruitment stands at 262/459 as of 6/10/2021.