Focal boosting in prostate cancer: risk modelling for individualized therapy
Karolina Guricova,
The Netherlands
OC-0259
Abstract
Focal boosting in prostate cancer: risk modelling for individualized therapy
Authors: Karolina Guricova1, Veerle Groen2, Floris Pos3, Evelyn Monninkhof4, Karin Haustermans5, Robert Jan Smeenk6, Jochem van der Voort van Zyp2, Cédric Draulans5, Sofie Isebaert5, Petra J. van Houdt1, Linda G. W. Kerkmeijer2,6, Uulke A. van der Heide1
1Netherlands Cancer Institute (NKI-AVL), Radiation Oncology, Amsterdam, The Netherlands; 2University Medical Center Utrecht, Radiation Oncology, Utrecht, The Netherlands; 3Netherlands Cancer Insitute (NKI-AVL), Radiation Oncology, Amsterdam, The Netherlands; 4University Medical Center Utrecht, Julius Center for Health Sciences and Primary Care, Utrecht, The Netherlands; 5University Hospital Leuven, Radiation Oncology, Leuven, Belgium; 6Radboud University Medical Center, Radiation Oncology, Nijmegen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
The FLAME trial showed that radiotherapy with iso-toxic
focal boosting to the intraprostatic lesion(s) in patients with intermediate and
high-risk prostate cancer improves disease-free survival (DFS). Due to the
strict adherence to organs at risk (OAR) constraints, a focal boost of D98%
> 90 Gy was reached only in 20% of the patients (median D98% 84.7 Gy). To
ensure the maximum treatment benefit without increasing OAR dose, more complex techniques
to improve high focal boost delivery may be needed. Therefore, it is important
to identify those patients who most likely require a high boost dose to achieve
control. In this study, we designed a risk model which predicts the 5-year DFS
based on individual clinical characteristics and the delivered boost dose.
Material and Methods
The model was designed using data of the FLAME trial of
526 patients with available clinical data who were
treated per protocol. The median follow-up was 72 months and clinical
failure occurred in 99 patients. The considered set of model parameters
consisted of the iPSA-value, cT-stage, ISUP grade group, age, use of hormonal
therapy and the delivered boost dose. Penalized Cox regression was used for
model development. Performance was evaluated with Harell’s C-index
(discrimination), the calibration curve and calibration-in-the-large. To
identify patients who would require a high boost dose to achieve control, we
calculated the predicted 5-year DFS, assuming they were treated to a standard
dose of 77 Gy. This was compared to predicted outcomes, assuming the same
patients received D98% of 95 Gy.
Results
The C-index of the model was 0.71 (95% CI: 0.69-0.72). The slope and
intercept of calibration curve were 0.97 and 0.011, respectively. The observed
versus predicted 5-year DFS was 84% vs. 83% in the control arm and 91% vs. 92%
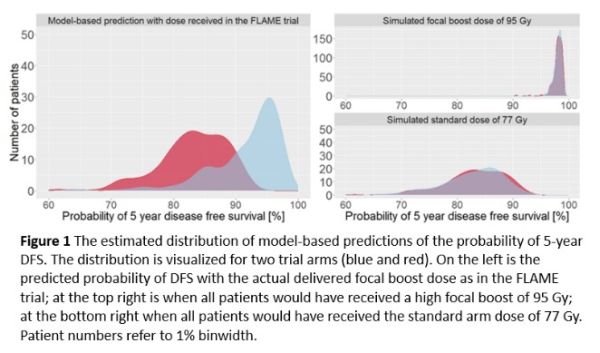
in the focal boost arm. The distribution of predicted outcomes for all patients
given the actual D98% they received in the trial is shown in Figure 1. On the
right side are the predictions if all would have received 77 Gy (bottom), or if
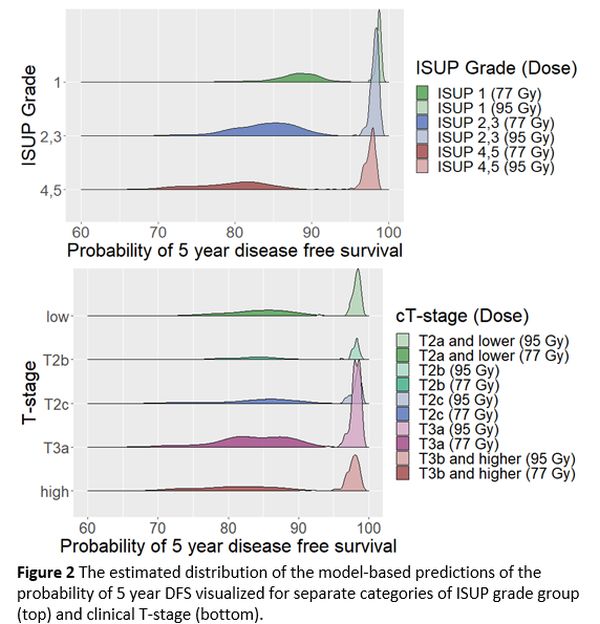
all would have had a boost dose of 95 Gy (top). Figure 2 shows the predictions
for separate categories of ISUP grade and T-stage. A trend towards a larger
improvement with a focal boost was observed for patients with high ISUP grade
disease. There was no trend observed for the impact of a focal boost for
different clinical T-stages.
Conclusion
We developed a prediction model for DFS in patients
with intermediate and high-risk prostate cancer treated with radiotherapy. The
model shows reasonable discrimination and good calibration. The model can be
used to identify patients who most likely require focal boosting through
evaluation of their predicted probability of 5-year DFS. The improvement in the
predicted DFS with a boost dose of 95 Gy, compared to the DFS with the actually
delivered boost dose, suggests the possible gain if alternative techniques of
high focal boost delivery are applied for these patients.