External validation of osteoradionecrosis NTCP models in head and neck cancer patients.
Niels den Haan,
The Netherlands
OC-0258
Abstract
External validation of osteoradionecrosis NTCP models in head and neck cancer patients.
Authors: Niels den Haan1, Sanne van Dijk1, Lisa van den Bosch1, Tineke van Zon-Meijer1, Anne van den Hoek1, Roel Steenbakkers1, Hans Verbeek1, Edwin Oldehinkel1, Arjan van der Schaaf1, Hans Paul van der Laan1, Hans Langendijk1
1UMCG, Radiotherapy, Groningen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Osteoradionecrosis
(ORN) of the mandible is an infrequent, yet a severely debilitating toxicity
following head and neck cancer (HNC) radiotherapy. The first ORN Normal
Tissue Complication Probability (NTCP) models for any grade (ORNI-IV) and grade IV
(ORNIV) have recently been developed
on a cohort of 1259
patients. The aim of this study was to externally validate these recently published multivariable
NTCP models in a large HNC patient cohort treated with (chemo-)radiotherapy.
Material and Methods
The
validation cohort consisted of 1154 HNC patients treated with definitive
(chemo)radiotherapy. Patients who underwent a mandibulectomy or had previous radiotherapy
in the HN area were excluded. Both cohorts used the ORN grading system
published by Tsai et al. who defined grade 4 ORN as ORN requiring major
invasive surgery. The original (logistic regression) NTCP models identified D30%
of the mandible and pre-radiotherapy (pre-RT) dental extraction as
independent factors for both ORNI-IV and ORNIV. The
original NTCP models were externally validated and the performance was
described with the AUC and R2. Additionally, the closed testing procedure (CTP)
was performed to test which model update was appropriate in our cohort: 1) by
calibration-in-the-large (re-estimation of model intercept), 2) recalibration
(re-estimation of intercept and slope) or 3) model revision (re-estimation of
all coefficients).
Results
The
prevalence of ORNI-IV and ORNIV in the validation cohort was
4% (n=44) and 1% (n=9), respectively, whereas the prevalence of ORNI-IV and
ORNIV in the development cohort was 13.7% and 5%. Similar as in the published
paper, all DVH parameters of the mandible were significantly associated to ORN
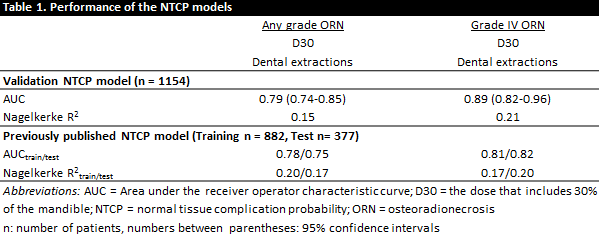
with univariate analyses. The external validation showed a similarly good and
comparable performance for the prediction of ORNI-IV and ORNIV
(Table 1). Additionally, the CTP did not detect major differences in the
validation cohort but recommended a re-estimation of the model intercept. The
intercept decreased from -6.85 to -8.90 for ORNI-IV and from -9.16
to -11.67 for ORNIV, while the coefficients of D30% and dental
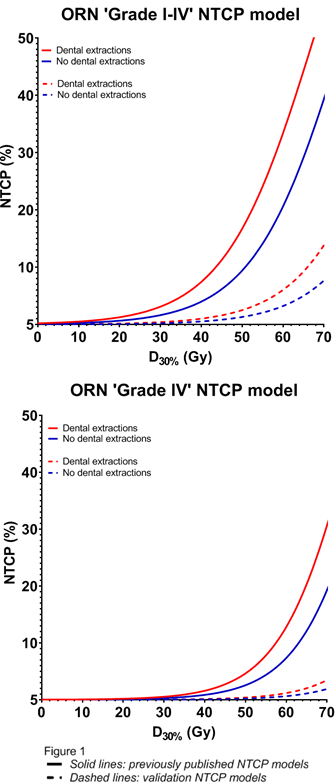
extraction remained the same. Please see
figure 1 for the NTCP models (validation and previously published NTCP model).
Conclusion
The
previously published ORN NTCP models with D30% of the mandible and
pre-RT dental extraction as independent factors were externally validated and
lead to similarly good and comparable performance for the prediction of ORNI-IV
and ORNIV. The CTP suggested a minor intercept update in order
to match our cohort, most likely due to the lower ORN prevalence in this
cohort. An explanation for this difference is subject of further investigation.
Overall, these models can be used to optimize radiotherapy treatment planning,
including patient selection for proton or photon therapy, aiming at prevention
of mandibular osteoradionecrosis.