Dysphagia at 1 year is associated with mean dose to the inferior section of the brainstem
OC-0255
Abstract
Dysphagia at 1 year is associated with mean dose to the inferior section of the brainstem
Authors: Eliana Maria Vasquez Osorio1, Azadeh Abravan1, Andrew Green1, Marcel van Herk1, Deborah Ganderton2, Andrew McPartlin3
1The University of Manchester, Division of Cancer Sciences, Manchester, United Kingdom; 2North Manchester General Hospital, Head and Neck Oncology and Voice, Manchester, United Kingdom; 3The Christie NHS Foundation Trust, Clinical Oncology, Manchester, United Kingdom
Show Affiliations
Hide Affiliations
Purpose or Objective
Dysphagia
is a common consequence of head and neck (HN) RT, which negatively affects
quality of life. Voxel-wise image-based data mining (IBDM) allows exploring the
relation between RT dose and treatment outcome without prior assumptions. Here,
we used IBDM to explore the relation between RT dose to normal HN anatomy and
dysphagia at 1 year after treatment, assessed using three validated outcome measures:
composite M.D. Anderson Dysphagia Inventory (MDADI), performance status scale for
normalcy of diet (HN-PSS), and water test (WT).
Material and Methods
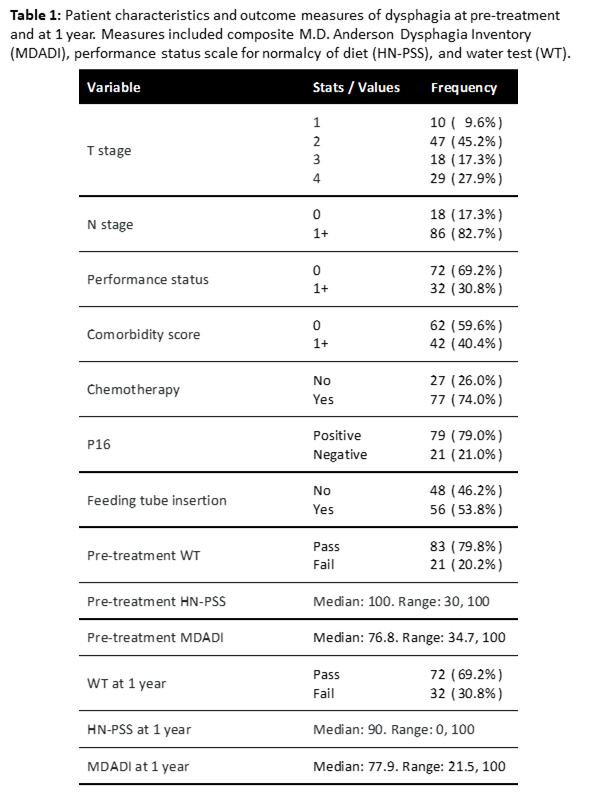
IBDM was applied to data from 104 oropharyngeal cancer
patients treated with definitive (Chemo)RT and assessed for swallow function
pre-treatment and at 1 year by a Swallow Assessment Specialist. We spatially
normalised all patient’s planning dose matrices (in equivalent dose at
2Gy/fraction, α/β=3Gy) to three arbitrary reference anatomies using a
combination of thin-plate splines deformation (for neck alignment) and NiftyReg.
To reduce target laterality bias, all patients were mirrored in the left-right
axis and mapped twice to the reference patient. Regions where the dose was
associated with outcome at 1 year were found by performing voxel-wise
statistics (t-test for WT, Spearman correlation for MDADI/HN-PSS) and permutation
testing (n=1000).
Mean and maximum doses of the overlap of the significant
regions for all outcomes were averaged across the three reference patients. Clinical
factors, treatment variables and pre-treatment measures for WT, HN-PSS and
MDADI (table 1) were used in multivariable analysis to predict WT (logistic
regression), HN-PSS and MDADI (linear regression) at 1 year. A clinical model was
found using backward stepwise selection for each outcome. Improvement of model
discrimination after adding the mean/max doses was quantified using Akaike
information criterion (AIC).
Results
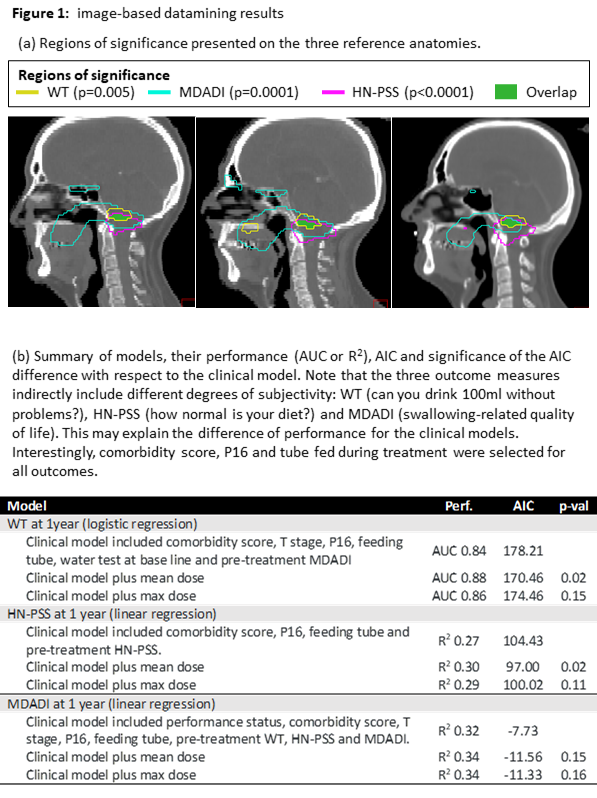
IBDM
revealed significant association between dose to distinct regions and the three
outcomes tested (p<0.005), overlapping around the inferior section of the
brainstem (figure 1). Models for WT and HN-PSS at 1 year were significantly
improved by including mean dose to the overlap region (p=0.02); this was not
the case for the MDADI model. Inclusion of max dose did not significantly
improve discrimination of any model.
Conclusion
Mean
dose to the inferior section of the brainstem is strongly associated with
dysphagia at 1 year following HN RT. The identified region is in proximity to swallowing
centres in the medulla oblongata, providing a possible mechanistic explanation.
Unexpectedly, no significant region was found close to the pharyngeal
constrictor muscles or salivary glands, despite dose to these structures being
predictive for dysphagia in previous studies. Mean, rather than max dose, was
most predictive, possibly indicating a parallel organ effect or a serial effect
in small substructures (masked by imperfect registration). Research is required
to derive a dose constraint for RT planning.