Improving brachytherapy needle ultrasound conspicuity with an echogenic coating
OC-0114
Abstract
Improving brachytherapy needle ultrasound conspicuity with an echogenic coating
Authors: Eric Brost1, Bradley Stish1, Chris Deufel1
1Mayo Clinic, Department of Radiation Oncology, Rochester, USA
Show Affiliations
Hide Affiliations
Purpose or Objective
This
study was aimed at improving the conspicuity of titanium high-dose rate (HDR)
brachytherapy needles under B-mode ultrasound imaging by applying a
commercially available echogenic surface coating (Sono-Coat™, Encapson,
Netherlands). The echogenic coating was
intended to improve needle visualization within regions of signal degradation that
can occur during prostate or gynecological HDR brachytherapy. Sono-Coat™ is a
commercial product designed to improve ultrasound visibility, particularly when
imaging objects which are nonparallel to the ultrasound transducer.
Material and Methods
17-gauge,
25 cm titanium HDR brachytherapy needles (Varian Medical Systems, USA) were
coated with Sono-Coat™, a coating composed of acoustically reflective
microspheres, over a 2 cm region starting from the needle tip. Three coatings
of variable thickness: M2 (25 um thickness), M3 (40 um), and M5 (64 um) were
compared against an uncoated control needle. The coated and uncoated needles
were imaged using B-mode ultrasound in a CIRS tissue equivalent prostate
phantom (CIRS Inc., USA) with a bk3000 (BK Medical, USA) unit and E14CL4b
transrectal probe. Needle conspicuity was assessed under three conditions: a single
needle implant, an implant with multiple needles between the probe and the needle
of interest, and an implant with simulated rectal gas. The simulated rectal gas
was introduced into images through taping medical gauze to the ultrasound probe
surface then wrapping the probe with a condom. All images were assessed qualitatively
for needle visibility and the presence of artifacts.
Results
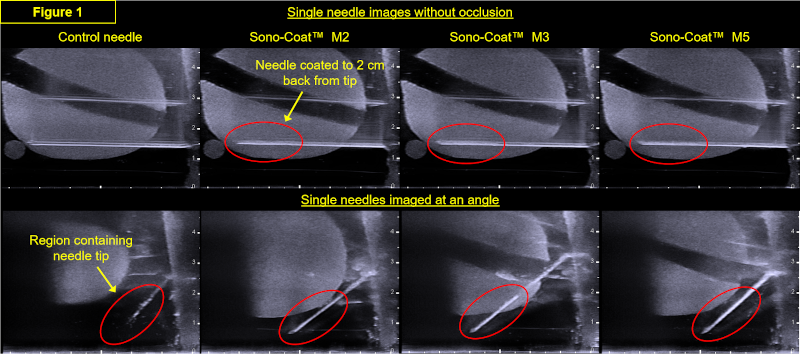
Under
ideal geometry, where the needle is implanted parallel to the transrectal
probe, the control needle and microsphere coated needle were equally visible (Figure
1, top panels). The microsphere coated needles produced noticeably less
reverberation artifact and appeared as a contiguous object, whereas the control
needle imaged as a bifurcated object along the body of the needle. When the
angle of incidence between the needle and probe was increased,
the visibility of the microsphere-coated needle was noticeably better than the
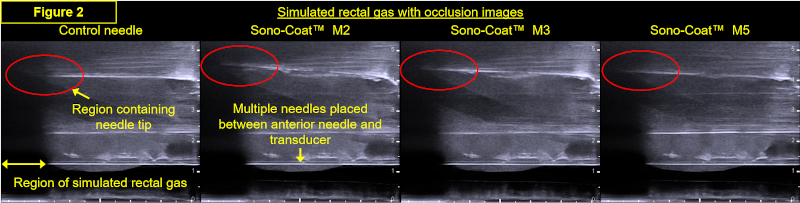
control needle (Figure 1, bottom panels). In the rectal gas simulation (Figure
2), the microsphere coating improved visibility into a region of signal
degradation, an effect that may be attributed to the redirection of ultrasound
waves by the microspheres from non-void regions towards the probe.
Conclusion
An
echogenic surface coating reduced reverberation artifacts and improved needle
visibility when brachytherapy needles were implanted at an angle to the
ultrasound probe or in the presence of B-mode signal degradation. The results
are consistent with the hypothesis that a microsphere coating can redirect
ultrasound waves to improve needle visibility when the signal-generating
ultrasound waves impinge nonparallel to the transducer. Testing is ongoing
within a cadaverous male pelvis.