Temporal lobe necrosis after proton therapy for skull base tumors and NTCP models evaluation
OC-0090
Abstract
Temporal lobe necrosis after proton therapy for skull base tumors and NTCP models evaluation
Authors: Giulia Riva1, Elisa Fiorina2, Iacopo Cavallo3, Silvia Molinelli4, Alessandro Vai4, Mario Ciocca4, Alberto Iannalfi3, Ester Orlandi3
1Centro Nazionale di Adroterapia Oncologica CNAO, Radiotherapy, PAVIA, Italy; 2Centro Nazionale di Adroterapia Oncologica CNAO, Clinical Department - Medical Physics Unit, PAVIA, Italy; 3Centro Nazionale di Adroterapia Oncologica CNAO, Clinical Department, Pavia, Italy; 4Centro Nazionale di Adroterapia Oncologica CNAO, Clinical Department - Medical Physics Unit, Pavia, Italy
Show Affiliations
Hide Affiliations
Purpose or Objective
The aims of this study were: i) to analyze the
relationship between radiation induced temporal lobe
necrosis (TLN) and dosimetric features in patients with skull base tumors treated
with pencil beam scanning proton therapy (PT); ii) to test available normal
tissue complication probability (NTCP) models.
Material and Methods
Clinical and dosimetric data of 110 adult
consecutive skull base chordoma and chondrosarcoma patients treated at CNAO
between September 2011 and July 2020 were retrospectively analyzed. A median dose of 70 Gy (RBE) (range 70-74 Gy (RBE))
was planned and delivered in 35-37 daily fractions. Current treatment planning
goal for TL was limiting the maximum dose to the hottests 2 cm3 (D2cc
) to 71 Gy (RBE). Magnetic Resonance Imaging (MRI) studies showing TLN at the first
occurrence were co-registered with the original planning images. TLN was
graded using Common Terminology Criteria for Adverse Events (CTCAE) v 5.0. The dosimetric parameters of TLs (Figure 1) were investigated for finding a correlation with the TLN’s occurrence and severity and
then included in NTCP univariate models. Their classification and
predictive performances were evaluated by means of goodness of fit (R2); Area Under ROC Curve
(AUC); accuracy, sensitivity and F-score.
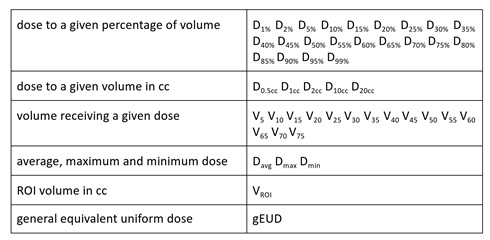
Figure 1 - Parameters extracted from DVHs for NTCP model evaluation.
Results
Median follow-up was 36 months (range 9-98 months).
Grade G1 TLN was reported in 26 patients (24%), while G2 in 14 cases (13%). No
TLN > G2 was recorded. 95% of patients had TLN
within 50 months from the end of treatment. Among the dosimetric
parameters analyzed, D0.5cc, D2cc and DMax
better correlate with the risk of TLN. The corresponding NTCP curves are
reported in Figure 2. For the G2 TLN models based on D0.5cc, D2cc
and DMax, R2 was 0.88, 0.95 and 0.92 whereas AUC was
0.80, 0.82 and 0.79, respectively. Moreover, when considering the TD
reproducing experimental G2 TLN occurrence, the
D2cc -based TLN model reached the best predictive performance
(accuracy = 0.71, sensitivity = 0.82, F-score = 0.33). Tolerance dose at 2 cm3
of TL for 5% and 20% probability of developing G2 TLN in 5 years were 62.9 Gy
(RBE) and 72 Gy (RBE), respectively, confirming the validity of the dose
constraint used for plan optimization.
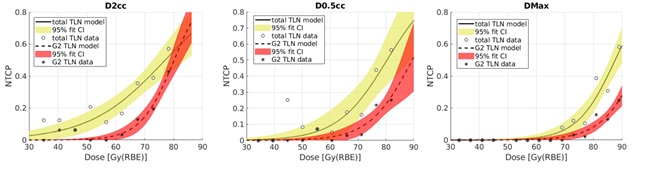
Figure 2 - Figure
1 - D2cc, D0.5cc, DMax NTCP models from univariate analysis. Shading limits the
region within the 95% confidence interval. Solid line-open circles (yellow) TLN
G > 0; dashed line-filled circles (red) TLN ≥ G2.
Conclusion
Patterns of TLN occurrence in patients with
skull-base chordoma and chondrosarcoma underwent PT were comparable with
literature data. High doses to very small TL volumes were the major predictors
of TLN. This analysis showed that the TL dose constraint, currently in use in
clinical practice, correctly predicted TLN G2 occurrence.