Early cost-effectiveness analysis of MR guided radiotherapy for colorectal liver metastases
Ellen Brunenberg,
The Netherlands
PO-1042
Abstract
Early cost-effectiveness analysis of MR guided radiotherapy for colorectal liver metastases
Authors: Joost Kleerebezem1, Ellen Brunenberg2, Karin Muller3, Janneke Grutters4
1Radboud UMC, Health evidence, Nijmegen, The Netherlands; 2Radboud UMC, Radiotherapy, Nijmegen, The Netherlands; 3RISO, Radiotherapy, Oncology, Deventer, The Netherlands; 4Radboud UMC, Health Evidence, Nijmegen, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
The
MR-Linac (MRL) is a recent innovation that allows for online re-planning, in
order to more accurately deliver radiotherapy to a targeted tumour area. However,
MR-guided radiotherapy devices are costly and require adjustments in protocol
and personnel compared to regular radiotherapy. In addition, the treatment is a
scarce option and thus not available to all patients. Therefore, in this study,
an early cost effectiveness analysis on online MR-guided radiotherapy (MRGRT) for
colorectal liver metastases is performed, to provide insights in
cost-effectiveness potential of MRGRT and, if possible, patient characteristics
that would make MRGRT treatment beneficial for some patients.
Material and Methods
A
Markov-state transition model with 1-year cycles was created to simulate a
hypothetical cohort of patients with colorectal liver metastases undergoing MRGRT
treatment versus conventional stereotactic body radiation therapy (SBRT) over
five years of follow up. Transition probabilities, healthcare costs and
utilities were extracted from available literature and Dutch guidelines. Outcomes were measured in net monetary
benefits (NMB) and incremental cost effectiveness ratios (ICER) using quality
adjusted life years (QALYs) as effectiveness measurement. Deterministic sensitivity
analysis was performed to assess model uncertainties, while scenario analyses
were performed to determine the potential health gains MRGRT can bring and thus
the parameters suitable for a threshold analysis. Subsequently, threshold
analyses were performed to calculate the necessary reductions in toxicity and
local recurrence (LR) rate for MRGRT to become cost-effective.
Results
In
the model, SBRT treatment resulted in a gain of 2.01 QALYs and 5-year costs of €7082 per patient. MRL treatment resulted in an
increase of €6103 in 5-year costs per patient, when no effect in local
recurrence, toxicity or survival was assumed. Scenario analysis showed a gain
of 0.0017 QALYs (ICER: € 3,574,420) and 0.0034 QALYs (ICER: € 1,787,210) when
toxicity rates were halved or completely eliminated, respectively. A gain of 0.1374
QALYs (ICER: € 42,874) and 0.2954 QALYs (ICER: € 18,997) was accomplished when LR
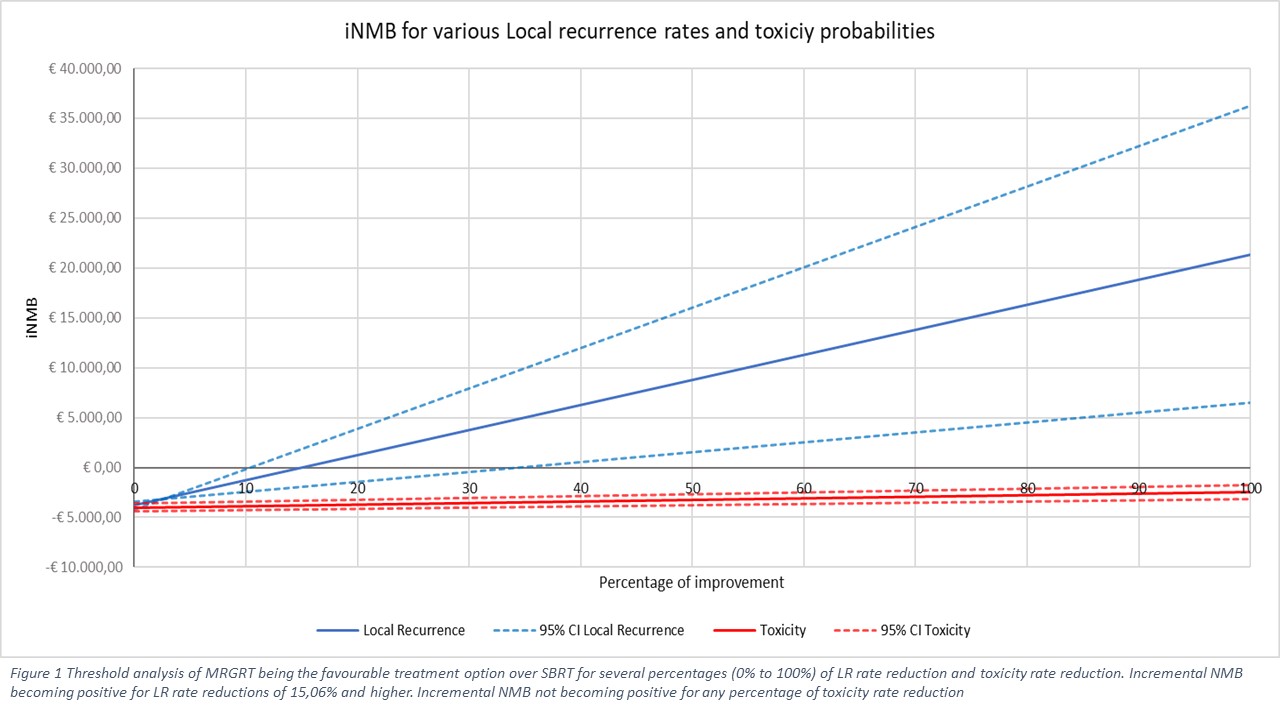
rates were halved or completely eliminated, respectively. Threshold analyses of
the toxicity and LR rate parameter (Figure 1) show that even complete
elimination of toxicity will not make MRGRT a cost-effective treatment.
However, MRGRT could become cost-effective if annual LR rates are reduced by 15%
or more.
Conclusion
Threshold
analyses showed that MRGRT can become a cost-effective alternative to SBRT when
LR rates are lowered with 15% compared to those related to SBRT. The effect of
toxicity on cost-effectiveness is minimal. MRGRT should be clinically tested
and results should be elaborately documented. There is a strong need for
extensive follow-up and registration studies to determine favourable patient
characteristics for each type of local treatment and to compare these
treatments based on their costs and effects.