Resource Requirements in Low- and Middle-Income Countries without Radiotherapy Facilities
Jonas Willmann,
Switzerland
PO-1036
Abstract
Resource Requirements in Low- and Middle-Income Countries without Radiotherapy Facilities
Authors: Jonas Willmann1, Sebastian M. Christ1
1University Hospital Zurich, University of Zurich, Department of Radiation Oncology, Zurich, Switzerland
Show Affiliations
Hide Affiliations
Purpose or Objective
Radiotherapy (RT) is one of three pillars of modern cancer care. Compared to surgery and systemic therapy, it is an inexpensive treatment modality. For many of the most common cancers, RT is essential for effective treatment. Yet, when planning and building cancer treatment resources, RT facilities are often underrepresented, especially in low- and middle-income countries (LMICs). Here, we determine the number of LMICs without RT facilities and try to quantify the infrastructure and human resource needs to close the gap.
Material and Methods
The most recent list of countries and their classification by income was obtained from the World Bank Group (WBG). Availability of RT facilities was taken from the Directory of Radiotherapy Centers (DIRAC) provided by the International Atomic Energy Agency (IAEA). Estimates for cancer incidence rates per country were obtained from the Global Cancer Observatory (GLOBOCAN). Requirements for staffing and infrastructure were estimated based on a quantitative algorithm developed and provided by the IAEA for differently sized RT centers [1].
Results
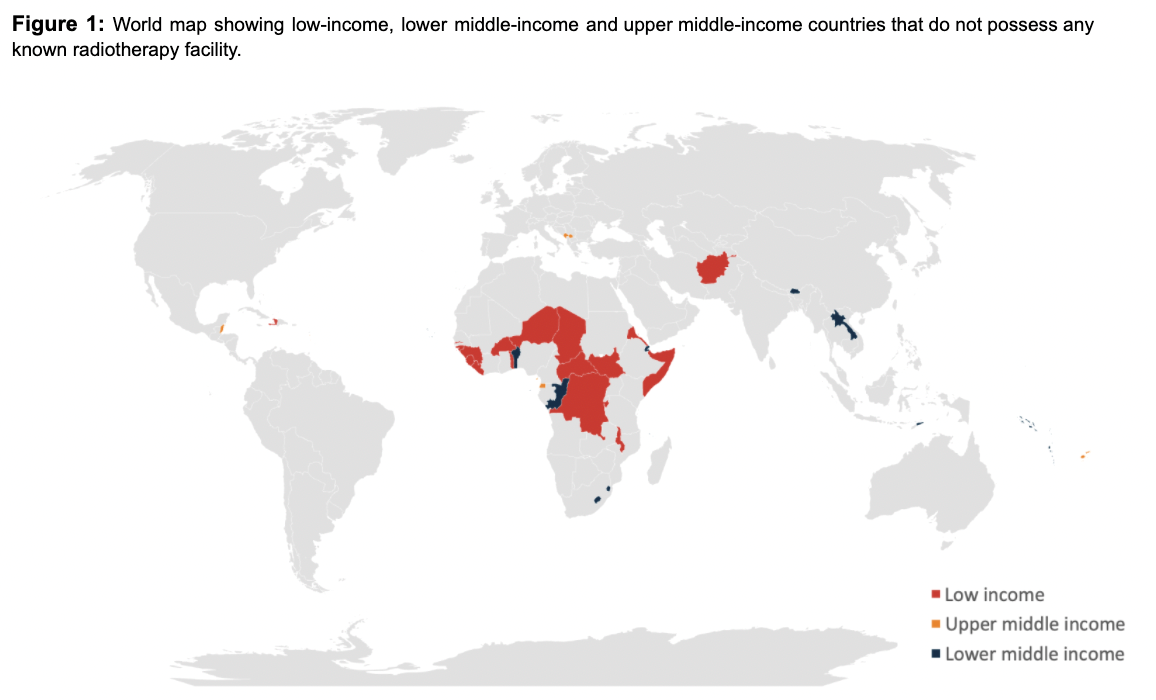
From the available data, 43 LMICs without any RT facilities were identified. The majority (n=20, 47%) of countries are located in Sub-Saharan Africa. Twenty-one (49%) countries are smaller nations with a population of under one million, many of whom (n=10, 23%) are island states in the East Asia and Pacific Region. One European country, Kosovo, is among the countries without any known RT facilities (see also Fig. 1).
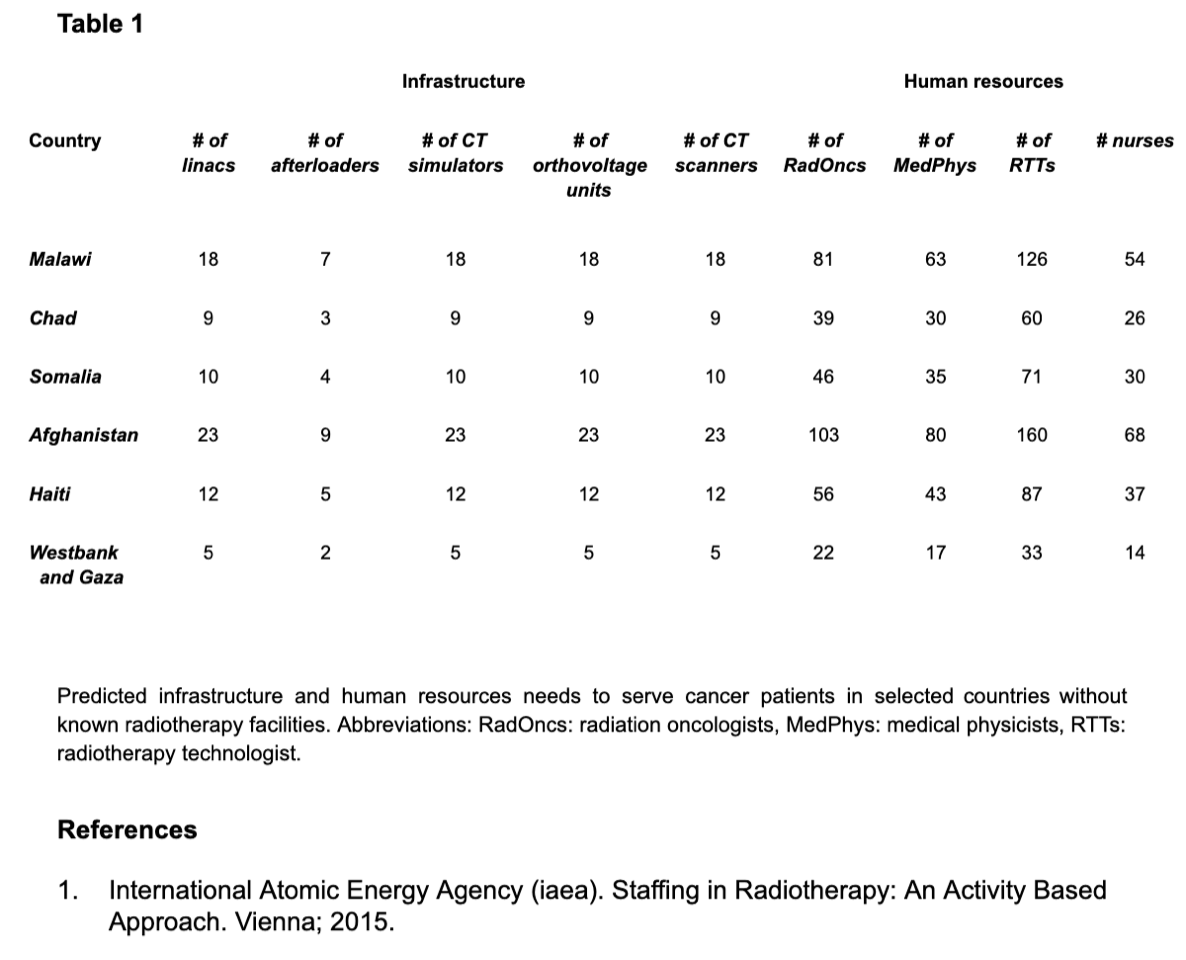
In terms of population, around ~197m people do not have access to RT facilities in their own country. Given the available cancer incidence data for these 43 LMICs, this amounts to an annual cancer case burden of ~136k, for some of which RT would be an effective treatment modality. The largest countries without RT departments in Africa are Malawi (pop: ~19m, annual cancer incidence: ~18k), Chad (pop: ~16m, annual cancer incidence: ~9k), and Somalia (pop: ~15m, annual cancer incidence: ~10k). Outside of Africa, the largest countries without RT facilities are Afghanistan (pop: ~38m, annual cancer incidence: ~23k), Haiti (pop: ~11m, annual cancer incidence: ~12k) and West Bank and Gaza (pop: ~7m, annual cancer incidence: ~5k). High-level, indicative estimates for current infrastructure and human resource needs for these six selected countries are shown in Table 1.
Conclusion
Even though RT is known to be an efficacious and cost-effective pillar in modern cancer care, hundreds of thousands of cancer patients in LMICs still do not have access to RT facilities in their country. Our findings indicate the need to further raise awareness and to encourage investment into the development of RT facilities to target these underserved populations. Quantifying the current gap in human resources and infrastructure requirements in countries without any RT facility might help health care policy makers and equipment providers to solicit investments to start to close the currently remaining gap.