Prediction models for rectal toxicity after brachytherapy in patients with pelvic cancer
Fariba Tohidinezhad,
The Netherlands
OC-0634
Abstract
Prediction models for rectal toxicity after brachytherapy in patients with pelvic cancer
Authors: Fariba Tohidinezhad1, Yves Willems1, Maaike Berbee1, Evert Van Limbergen1, Frank Verhaegen1, Andre Dekker1, Alberto Traverso1
1Maastricht University Medical Center, Department of Radiation Oncology (Maastro Clinic), Maastricht, The Netherlands
Show Affiliations
Hide Affiliations
Purpose or Objective
Over the last decades, Brachytherapy (BT) with or
without supplemental External Beam Radiotherapy (EBRT) has demonstrated
excellent effectiveness in localized advanced pelvic cancers, especially in
patients with prostate and cervical malignancies. In recent years, quality of
life after BT has become a concerning issue among physicians and patients for
selecting the optimal treatment modality. Although brachytherapy allows for
rapid dose falloff, the rectal wall still receives high doses of radiation due
to the proximity to the tumor. Literatures show 5-7% of the patients complain
of grade II or higher rectal toxicities. Better knowledge of the dose-toxicity relationship is essential for safe
dose escalation to minimize rectal toxicity without impairing therapeutic
benefit. This study was aimed to abstract and evaluate the studies which have
developed a prediction model for rectal toxicity after BT in patients with
pelvic cancer.
Material and Methods
To identify
relevant studies since 1995, MEDLINE was searched on August 31, 2021 using the
terms related to “pelvic cancer sites”, “rectal toxicity”, “prediction model”,
and “brachytherapy”. Two independent reviewers screened the citations. The
papers were excluded if only a subset of patients received BT,
entering/removing predictors were not reported, or mixed outcomes were used as
the primary endpoint. Risk of bias associated with methodological conduct was
assessed using the Prediction model Risk Of Bias ASsessment Tool (PROBAST).
Results
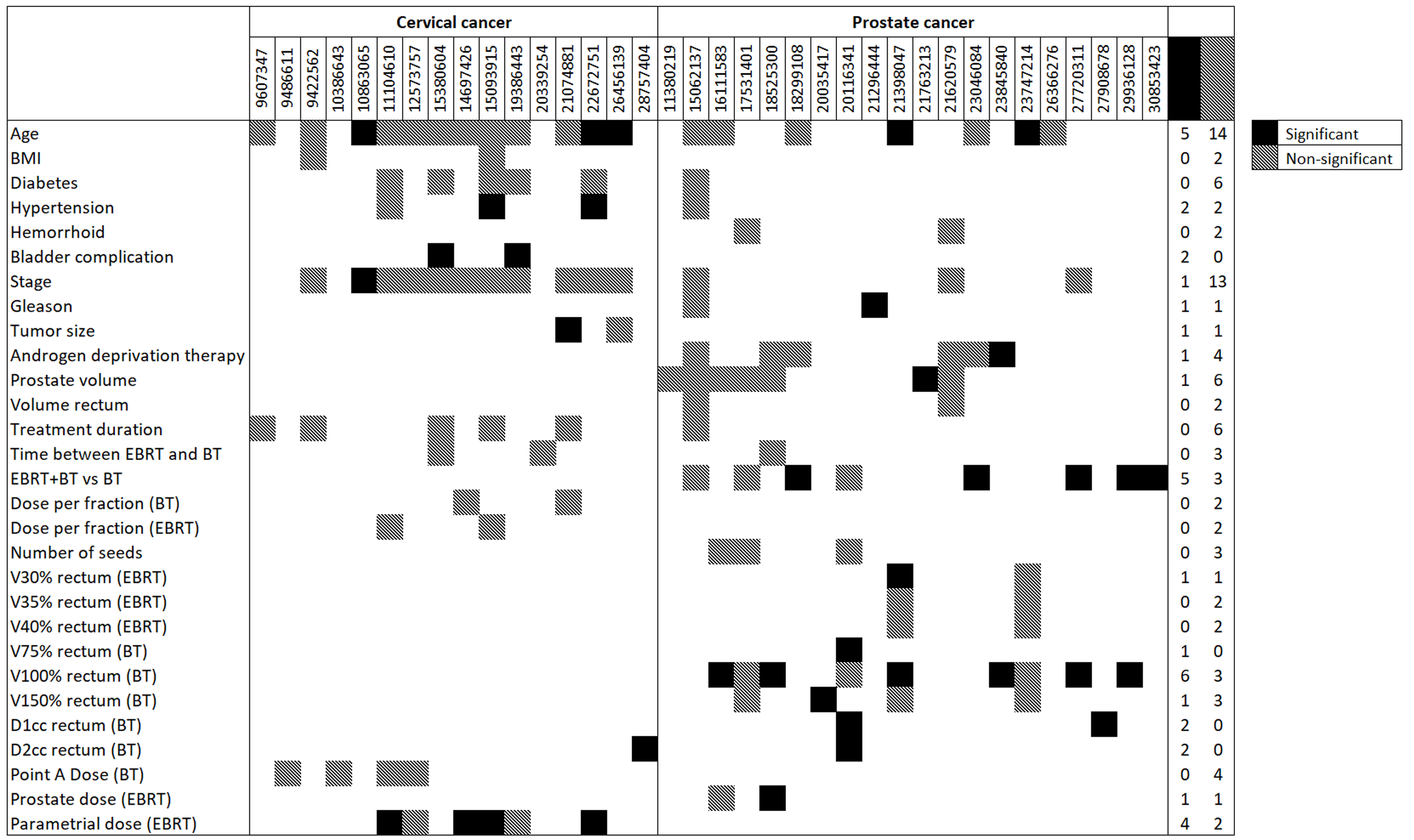
Forty-three
prediction models featuring 117 distinct predictors (Figure 1) were published
between 1998 and 2019. A total of 20 (47%) and 21 (49%) models were developed
for prostate and cervical cancers, respectively. One study included elderly
rectal cancer patients and one study developed a model for patients with
different gynecological cancers. Rectal toxicity varied significantly between
studies (3%-39% for prostate and 7%-47% for cervical cancers). Thirty-nine
(91%) of the studies performed combined EBRT and BT and 11 (52%) studies
included the gynecology cancer patients with the history of chemotherapy. Radiation
Therapy Oncology Group (RTOG) and Common Terminology Criteria for Adverse
Events (CTCAE) were used in 61% and 19% of the studies as the outcome measuring
standard. Regression, support vector machine, and neural network were used in
40 (93%), 2 (5%), and 1 (2%) studies, respectively. Only five studies (12%)
reported the area under the receiver operating characteristic curve
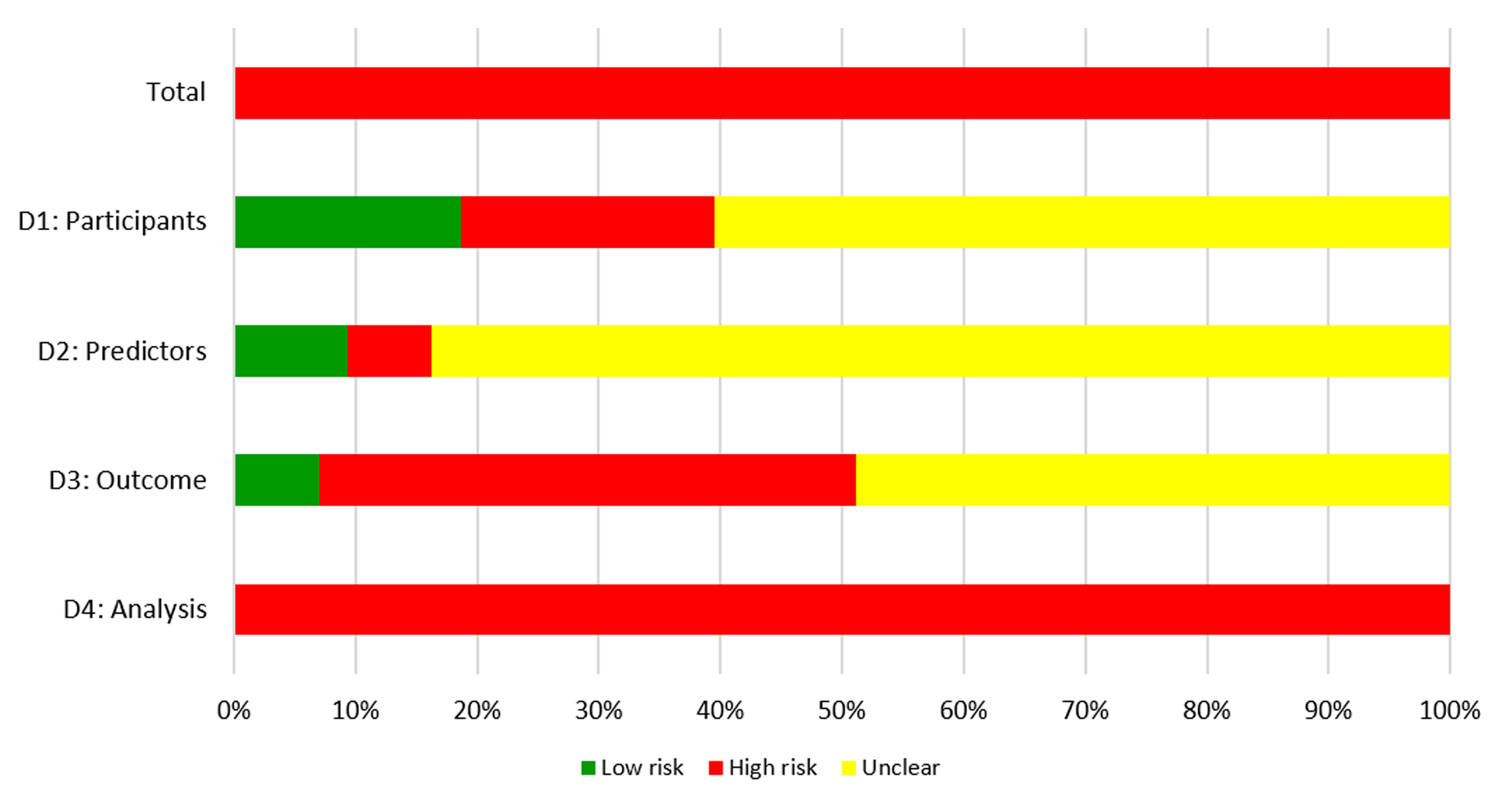
(0.58-0.91). All studies were judged to be at high risk of bias mainly due to
methods of analysis (Figure 2).
Conclusion
The currently available models appear to be of
suboptimal quality and therefore caution should be considered for using these
models in clinical practice. Future model development studies should adhere to
methodological guidelines because unreliable models could misguide clinical
decision making. The identified predictors in this study can be used as the
potential predictors in future models.