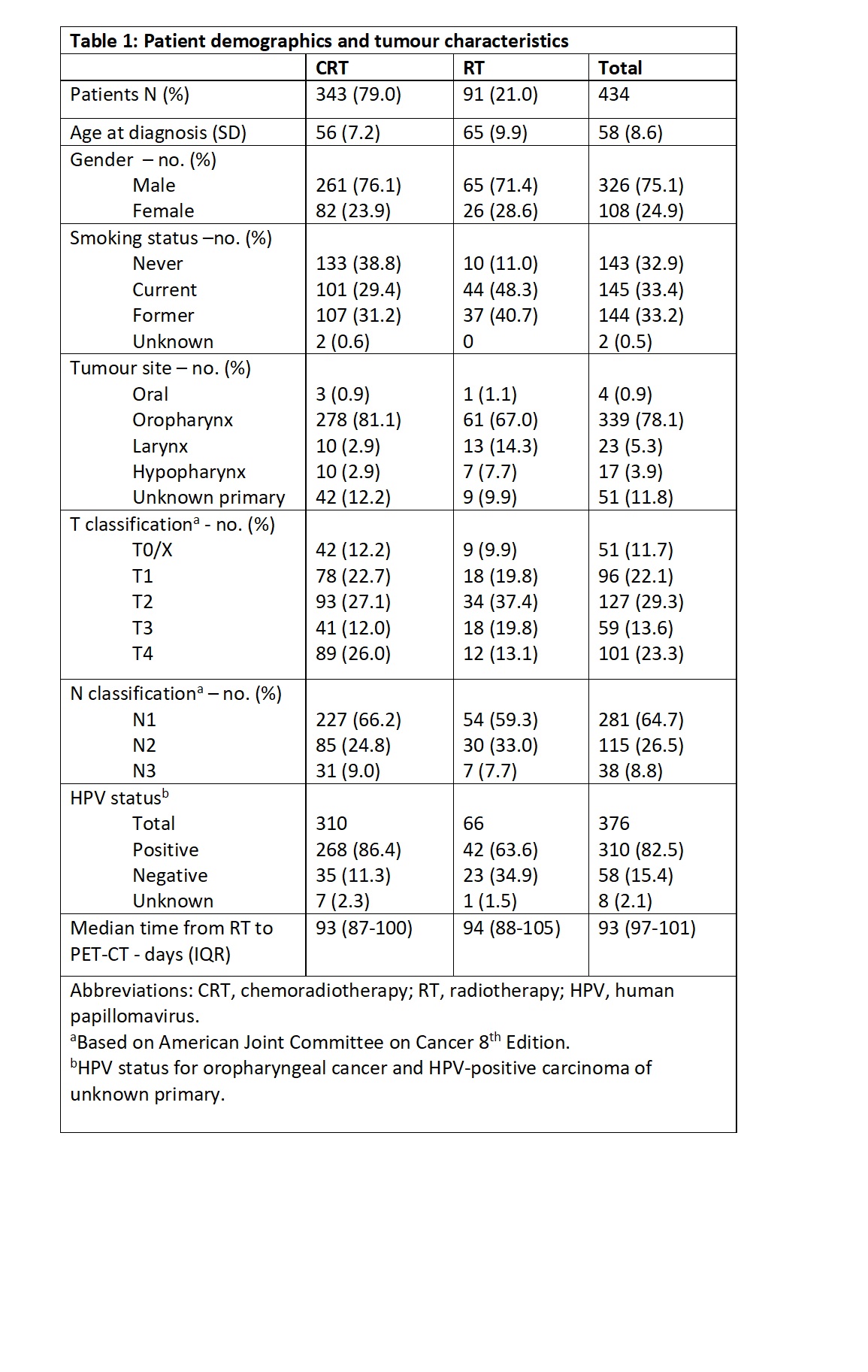
434
HNSCC patients were identified, patient and tumour characteristics are detailed
in Table 1. Median time from end of RT to PET scan was 93 (IQR 97-101) days. Median
follow-up was 42.7 (IQR 30.8-60.0) months.
343
(79%) patients received CRT and 91 (21%) had RT alone.
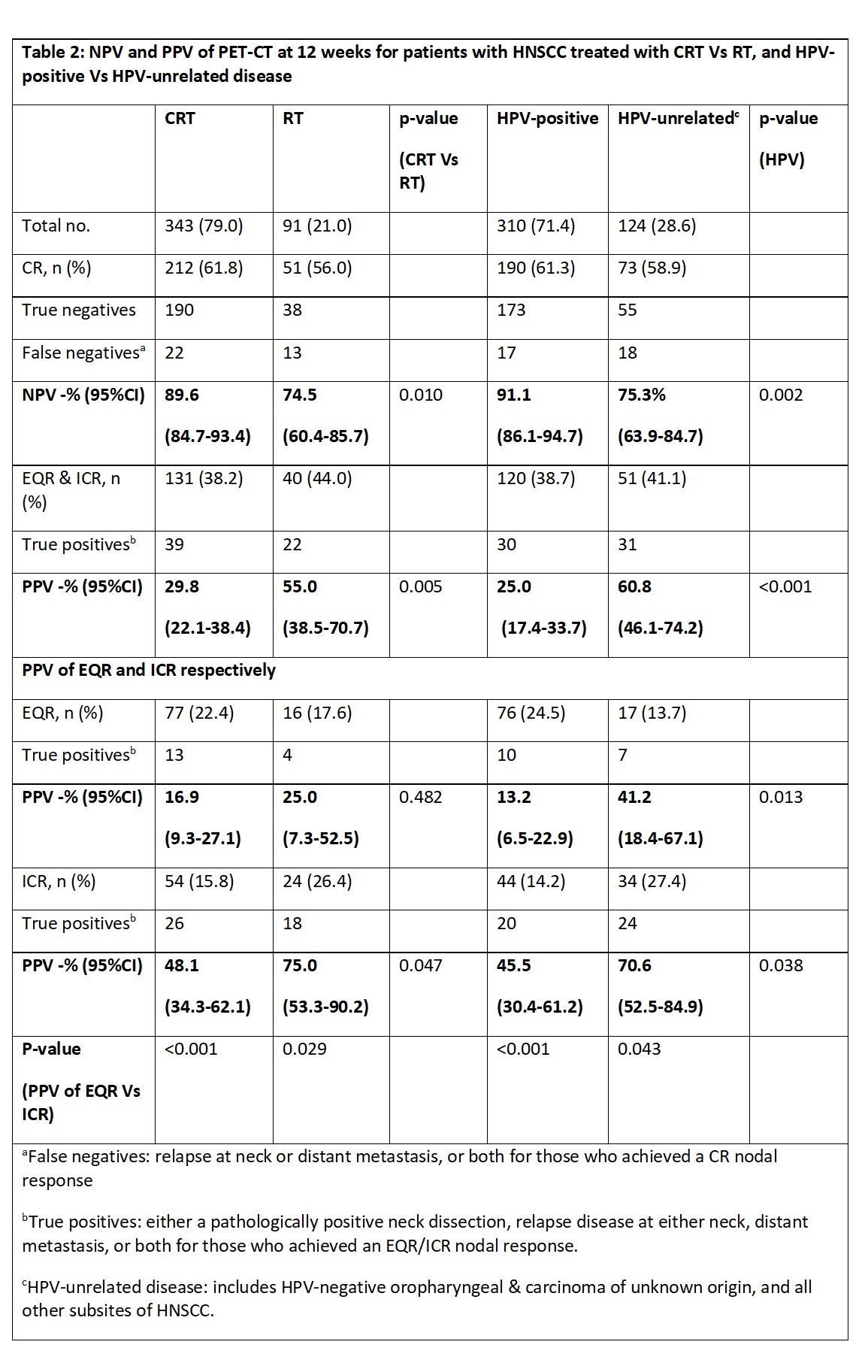
In
the CRT group (n=343), 212 (61.8%) achieved a CR; 131 (38.2%) less than CR with
39 cases of recurrence, thus the PPV of PET-CT for CRT was 29.8% (95% CI 22.1-38.4), see Table 2.
In the RT-only group (n=91), 51 (56%)
achieved a CR; 40 (44%) a less than CR with 22 cases of recurrence. Hence the PPV of
PET-CT was 55.0 (95% CI 38.5-70.7) -significantly
higher than the PPV of the CRT group, p=0.005.
When stratifying for HPV status, 310
(71.4%) patients had HPV-positive and 124 (28.6%) HPV-unrelated HNSCC.
Of the
310 HPV-positive group, 190 (61.3%) patients achieved a CR; 120 (38.7%) less than CR with 30 cases of recurrence. Thus the PPV of PET-CT
was 25% (95CI%
17.4-33.7).
In the HPV-unrelated HNSCC group (n=124),
73 (58.9%) achieved a CR; 51 (41.1%) less than CR with 31 cases of recurrence. The
PPV of PET-CT was 60.8% (95%CI 46.1-74.2). This is significantly higher than
the PPV of the HPV-positive group, p<0.001.
Of the 120 HPV-positive patients who achieved
a less than CR; 76 (24.5%) achieved EQR with 10 cases of relapse; and 44 (14.2%)
ICRs, of which 20 patients had recurrence. PPV for PET-CT was 13.2% (95%CI
6.5-22.9) and 45.5% (95%CI 30.4-61.2) for EQR and ICR groups, respectively.
Within the HPV-positive cohort, the PPV was significantly lower for the EQR
compared to the ICR group, p<0.001.
PPV for HPV-positive group was
significantly lower than that of the HPV-unrelated group for both EQR and ICR
groups, p=0.013 and p=0.038, respectively.